Researchers report that some people who experience heart failure have less biodiversity in their gut or have elevated gut metabolites, both of which are associated with more hospital visits and greater risk of death. A team led by scientists at the Georgetown University School of Nursing & Health Studies published their study, “The heart and gut relationship: a systematic review of the evaluation of the microbiome and trimethylamine-N-oxide (TMAO) in heart failure,” in Heart Failure Reviews.
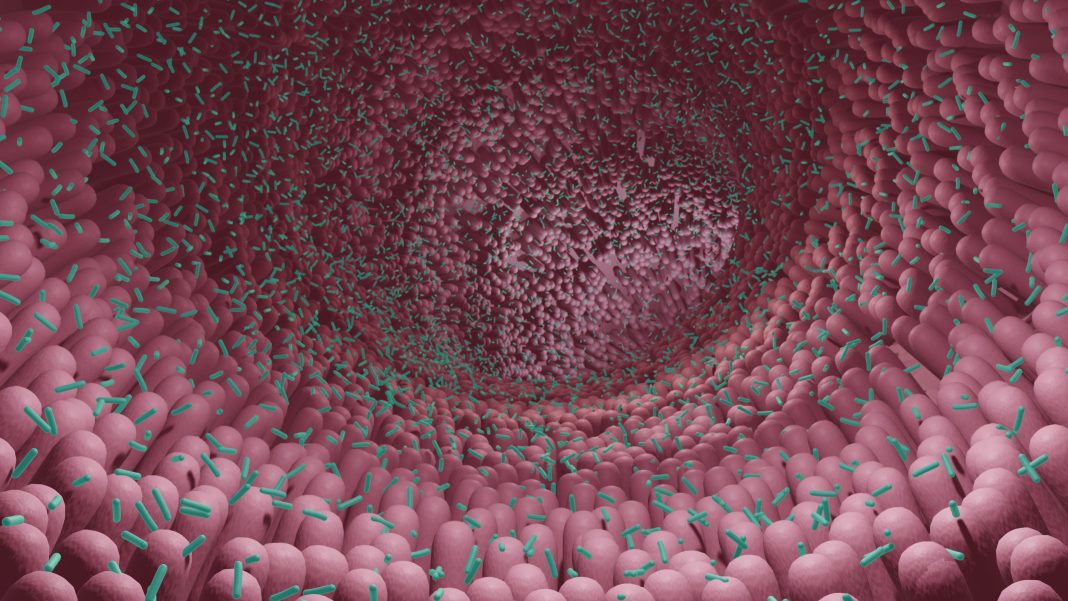
The gut microbiome is a delicately balanced ecosystem comprised primarily of bacteria as well as viruses, fungi, and protozoa. The microbiome can affect cardiovascular disease, which is a leading cause of death in the U.S.; heart failure, affecting over six million Americans annually, is often the end-stage of progressive cardiovascular disease.
For their overview, the researchers looked at seven years of genetic, pharmacologic, and other types of research findings from around the world to generate a wide perspective on how the microbiome can influence heart failure. The investigators zeroed in on one harmful metabolite, trimethylamine-N-oxide (TMAO), that can be produced by churning gut microbiota when full-fat dairy products, egg yolks, and red meat are consumed.
“There is an expanding body of research on the bidirectional relationship of the human gut microbiome and cardiovascular disease, including heart failure (HF). Researchers are examining the microbiome and gut metabolites, primarily trimethylamine-N-oxide (TMAO), to understand clinically observed outcomes. This systematic review explored the current state of the science on the evaluation and testing of the gut biome in persons with HF,” write the investigators.
“Using electronic search methods of Medline, Embase, CINAHL, and Web of Science, until December 2021, we identified 511 HF biome investigations between 2014 and 2021. Of the 30 studies included in the review, six were 16S rRNA and nineteen TMAO, and three both TMAO and 16S rRNA, and two bacterial cultures. A limited range of study designs were represented, the majority involving single cohorts (n = 10) and comparing individuals with HF to controls (n = 15). Patients with HF had less biodiversity in fecal samples compared to controls.

“Further longitudinal and multi-centered studies are required to inform interventions to promote clinical decision-making and improved patient outcomes.”
“To diagnose and manage heart failure we rely on certain findings and test results, but we do not know how poor heart function influences the activities of the gut, including the absorption of food and medications,” says Kelley Anderson, PhD, associate professor of nursing at Georgetown and corresponding author of the study. “There is now an appreciation of a back-and-forth relationship between the heart and elements in the gut, as clearly the heart and vascular system do not work in isolation–the health of one system can directly influence the other, but clear connections are still being worked out scientifically.”
The investigators parsed 511 research articles published between 2014 and 2021 that connected the microbiome with heart failure and winnowed their focus to the 30 most relevant articles. In recent years, more advanced technology, particularly tools that can closely examine the biological roles of DNA and RNA in the body, provided more detailed insights into the gut/heart relationship and those studies were of particular interest.
The researchers could not pinpoint the effects of diet on the interplay between the microbiome and the cardiovascular system due to a lack of strong data from the studies they reviewed. The investigators noted that nutrition is an important component of overall cardiovascular health, so having the opportunity to explore the impact of diet in relation to the microbiome is a promising area for future research efforts.
In terms of possible interventions to mitigate negative impacts of the microbiome on heart disease, Anderson noted that there are ongoing studies evaluating the use of antibiotics, prebiotics, and probiotics, all of which can impact the microbiome, as well as intestinal binders that glom on to and help shuttle harmful elements out of the gut.
“We are currently developing a forward-looking study to evaluate the microbiome in patients with heart failure. We are particularly interested in the symptomatic experience of patients with end-stage heart failure as well as disease-related weight loss and wasting during this stage of cardiovascular disease,” says Anderson.