Soft-tissue sarcomas are very challenging to treat. One reason is because knowledge of the sarcoma microenvironment composition is limited. Therefore, successful interventions for some solid tumors that target the tumor microenvironment may not be applicable.
Now, researchers have used single-cell RNA-seq to characterize the immune composition of an undifferentiated pleiomorphic sarcoma mouse model. They discovered that soft-tissue sarcomas produce a protein that switches immune cells from tumor-attacking to tumor-promoting. The study could lead to improved treatments for soft-tissue sarcomas.
This work is published in Cell Reports in the article, “Single-cell RNA-seq of a soft-tissue sarcoma model reveals the critical role of tumor-expressed MIF in shaping macrophage heterogeneity.”
“Tumors also recruit immune cells,” said Ilenia Guarnerio, PhD, a research scientist with Cedars-Sinai Cancer and assistant professor of radiation oncology and biomedical sciences. “These immune cells should be able to recognize and attack the tumor cells, but we found that the tumor cells secrete a protein that changes their biology, so instead of killing tumor cells they actually do the opposite.”
Soft-tissue sarcoma is a rare type of cancer that forms in the muscle, fat, blood vessels, nerves, tendons, and joint lining. It most commonly occurs in the arms, legs, and abdomen, and kills more than 5,000 people in the United States each year, according to the American Cancer Society.
The researchers used single-cell RNA-seq to characterize the immune composition of an undifferentiated pleiomorphic sarcoma mouse model. In comparing samples of a variety of soft-tissue sarcomas in humans and laboratory mice, Guarnerio and her team noted that most of these tumors have an abundance of myeloid cells in their microenvironment.
“It was striking that such a large percentage of the immune cells were myeloid cells, and we thought that since they obviously weren’t killing the tumor cells, they must be doing something to promote tumor growth,” said Stephen Shiao, MD, PhD, division director of the division of radiation biology and co-leader of the Translational Oncology Program. “And indeed, our analysis of tumor samples showed that many of the myeloid cells had adopted a tumor-promoting function.”
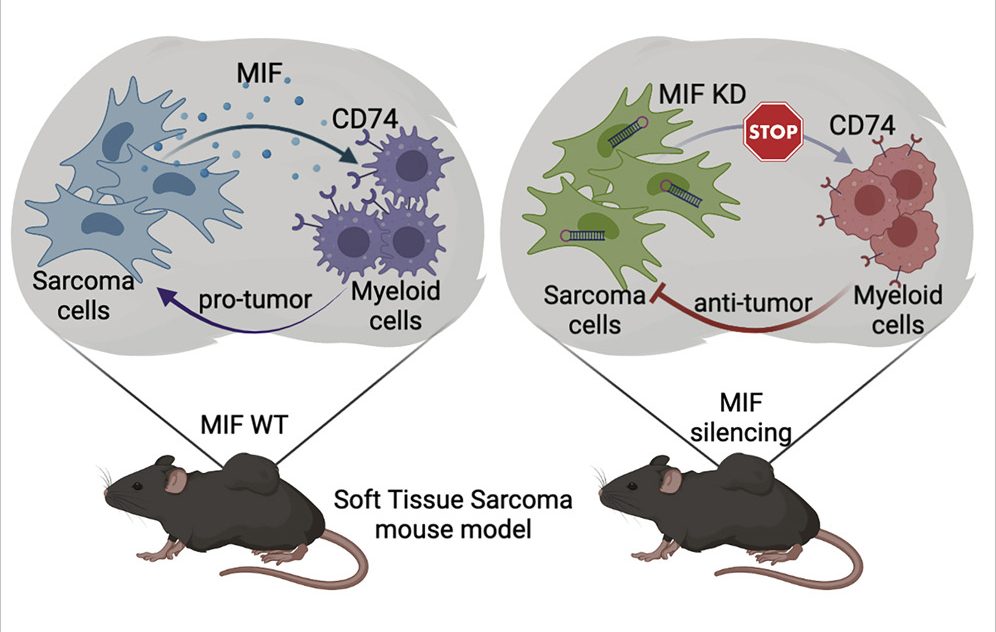
To find out what was causing this change, investigators examined the proteins secreted by the tumor cells and the receptors on the surface of the myeloid cells. “We examined the cross-talk between these two populations of cells,” Guarnerio said. “We found that the tumor cells expressed high levels of a protein called macrophage migration inhibitory factor [MIF], and that the myeloid cells had receptors to sense the MIF proteins. This makes them switch their biology and promote, rather than block, tumor growth.”
When the investigators generated tumors from cancer cells that didn’t express MIF, myeloid cells were able to penetrate the tumors and tumor growth was reduced.
“This means the myeloid cells might have attacked the tumors directly, or might have activated other immune cells, for example T cells, to attack the tumors,” Guarnerio said.
The investigators believe this information could be used to create novel therapies against soft-tissue sarcoma. A medication designed to stop cancer cells from expressing MIF could be tested in combination with existing therapies, for example, to see if it improves outcomes for patients.
“The majority of studies in cancer biology and immunotherapy have been done on carcinoma, the most common type of cancer,” Guarnerio said. “Much work has been done to describe which types of immune cells infiltrate these tumors and how carcinoma cells interact with immune cells, but there is almost no research on sarcomas. We need to continue our investigation so that we understand the roles of many other cells—T cells and B cells, for example—and how all the players work together.”