Source: Havard Stem Cell Institute
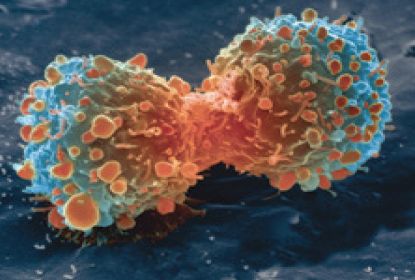
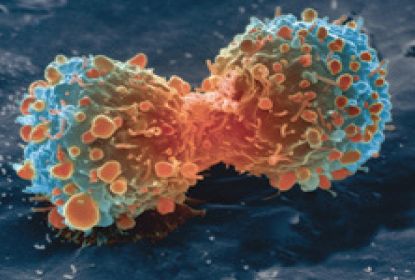
A member of a protein family that has previously been thought to play a tumor-suppressive role in breast cancer may in fact be key to the maintenance of self-renewing cancer stem cells (CSCs) that drive one of the most aggressive form of the disease. Studies by a Cleveland Clinic team, headed by Justin Lathia, Ph.D., and Ofer Reizes, Ph.D., found that the gap junction (GJ) protein connexin 26 (Cx26) forms part of a signaling complex that drives CSC maintenance in triple-negative breast cancer (TNBC) via a pathway that isn’t related to GJ function.
The results indicate that Cx26 and its signaling complex could represent a new target for inhibiting CSC survival and spread in TNBC. “These findings challenge the paradigm that connexins are tumor suppressors in TNBC and reveal a unique function for Cx26 in regulating the core self-renewal signaling that controls CSC maintenance,” the team writes in a paper published today in Nature Communications, which is entitled, “Cx26 Drives Self-Renewal in Triple-Negative Breast Cancer via Interaction with NANOG and Focal Adhesion Kinase.”
“Additional research is needed, but this discovery suggests that inhibiting Cx26 and the related pathway may be a promising new strategy for stopping or preventing TNBC stem cells from self-renewing and spreading,” Dr. Lathia suggests. “It may also offer a target for diagnostic testing that helps clinicians predict health outcomes and relapse-free survival for patients with a specific cancer type.”
TNBC is defined by the lack of estrogen receptor, progesterone receptor, and Her2/neu receptor expression, and has the poorest prognosis of all the forms of breast cancer, the researchers explain. The disease is characterized by persistent tumor growth, resistance to therapy, and metastasis, which are largely believed to be driven at least in part by self-renewing CSCs.
Connexins are a family of GJ proteins that facilitate direct cell-to-cell communication, and also function as single membrane channels or as signaling hubs. GJ communication channels have previously been reported to demonstrate tumor-suppressive functions, including in TNBC, the researchers note. Similarly, a tumor-suppressive role for connexins has also been suggested. “In the context of cancer, connexins are widely considered to be tumor suppressors in many cancer models.” More recent evidence is challenging this general tenet, however, and suggests that connexins may have protumorigenic functions, including tumor progression and metastasis.
Cx26 is one of two connexion subunits that are expressed predominantly in breast tissue. Prior studies have described connexins to be both pro- and antitumorigenic in breast cancer, although, as the Cleveland Clinic researchers state, “Most studies to date suggest a tumor-suppressive role for Cx26 in early breast cancer progression based on evidence that Cx26 is frequently absent or downregulated in human breast cancer cell lines and human primary tumors.”
In contrast, clinical observations have demonstrated what the authors term a strong correlation between increased Cx26 expression in breast cancer samples taken after chemotherapy or surgery and reduced survival. Other studies have linked Cx26 expression with increased lymphatic vessel invasion, increased tumor size, and poor prognosis in human breast cancers.
Although a role for connexions in CSCs in TNBC hasn’t yet been identified, work by the Cleveland Clinic researchers had previously identified a role for a different connexin, Cx46, in maintaining CSCs in another cancer, glioblastoma, “suggesting that different connexin family members may play distinct roles.” Based on their previous work and other observations, the team then “hypothesized that a subset of connexions may regulate CSC maintenance in TNBC independent of their role in cell-cell communication.”
The researchers first carried out an analysis of multiple TNBC datasets, which confirmed that Cx26 was the most highly expressed connexion in TNBC, and in particular in CSCs. Studies in cultured cancer cells then showed that silencing Cx26 gene expression decreased expression of NANOG, a key transcription factor that is important for CSCs, and reduced the self-renewal capacity of CSCs. Cx26-silenced cells were also less capable of initiating new tumors. Conversely, forcing overexpression of Cx26 in non-CSC cancer cells was enough to induce CSC marker expression, increase self-renewal, and promote tumor initiation.
Interestingly, subcellular analyses suggested that in TNBCs, Cx26 wasn’t expressed in the plasma membrane where connexins form GJs, but was instead localized in the cytoplasm and the nuclear envelope. These findings “support a GJ-independent role of Cx26 that is critical to maintain self-renewal and tumor initiation capacity in TNBC CSCs.”
Further analyses of TNBC lines confirmed that Cx26 physically interacts with NANOG and FAK to generate a complex that is localized adjacent to the nucleus. This complex was found to play “an essential role in TNBC CSC self-renewal and tumor initation capacities.”
“Our studies reveal a new GJ-independent role for Cx26 in the maintenance of CSC self-renewal in TNBC,” the authors conclude. “Taken together, our studies reveal a unique signaling complex containing Cx26, NANOG, and FAK that may be amenable for targeting and compromising TNBC CSC maintenance.” They add that, “A Cx26/NANOG/FAK signature might also be clinically useful as a new prognostic factor informative of TNBC patient outcome.”
“TNBC is resistant to treatment and has a high recurrence rate,” Reizes notes. “This aggressive subtype accounts for about 15% to 20% of breast cancers. Our findings are at an early stage, but we are hopeful that targeting these cancer stem cells will lead to new treatments to allow women to be treated successfully and improve their outcomes.”