Thrombolytic drugs are the main treatment for stroke, but they have often not been recommended for people who have an aneurysm in their brains that has not ruptured. A new study (“Risk of Aneurysm Rupture After Thrombolysis in Patients With Acute Ischemic Stroke and Unruptured Intracranial Aneurysms”), published in Neurology, finds that these aneurysms rarely burst after treatment with thrombolytics, so the drugs may be safe for use.
“Unruptured intracranial aneurysms (UIAs) are considered to be a relative contraindication for intravenous thrombolysis (IVT) in acute ischemic stroke (AIS). However, there is currently limited data on the risk of UIA rupture following IVT. Our objective was to assess whether IVT for AIS can lead to a UIA rupture and intracranial hemorrhages (ICHs) in patients with unruptured UIAs,” write the investigators.
“Prospective cohort study of consecutive patients treated in a comprehensive stroke center between 2005 and 2019. We assessed radiology reports and records at the Finnish Care Register for Health Care to identify patients with UIAs among all AIS patients treated with IVT at the center. We analyzed patient angiograms for aneurysm characteristics and other brain imaging studies for ICHs after IVT. The main outcome was in-hospital ICHs attributable to an UIA rupture after IVT. Secondary outcomes were in-hospital symptomatic ICHs (ECASS-2 criteria, i.e., NIH Stroke Scale score increase of ≥ 4 points) and any in-hospital ICHs.
“A total of 3,953 patients were treated with IVT during the 15-year study period. One hundred thirty-two (3.3 %) of the 3,953 AIS patients had a total of 155 UIAs (141 saccular and 14 fusiform). The mean diameter of UIAs was 4.7 ± 3.8 mm, with 18.7% being ≥ 7 mm and 9.7% ≥ 10 mm in diameter. None of the 141 saccular UIAs ruptured following IVT. Three patients [2.3%, 95% confidence interval (CI) 0.6-5.8%] with large fusiform basilar artery UIAs suffered from a fatal rupture at 27 hours, 43 hours, and 19 days after IVT. All three were administered anticoagulation treatments following IVT and anticoagulation took effect during the UIA rupture. Any ICHs and symptomatic ICHs were detected in 18.9 % (95% CI 12.9-26.2%) and 8.3% (95% CI 4.4-13.8%) of all AIS patients, respectively.
“IVT appears to be safe in AIS patients with saccular UIAs, including larges UIAs (≥10 mm). Anticoagulation after AIS in patients with large fusiform posterior circulation UIAs may increase the risk of aneurysm rupture.”
Results indicate that more patients may receive thrombolytic therapies
“These results are exciting because they may expand the population who can receive these thrombolytic therapies that can prevent death and disability for people with strokes,” said study author Jyri Juhani Virta, MD, PhD, of the University of Helsinki in Finland.
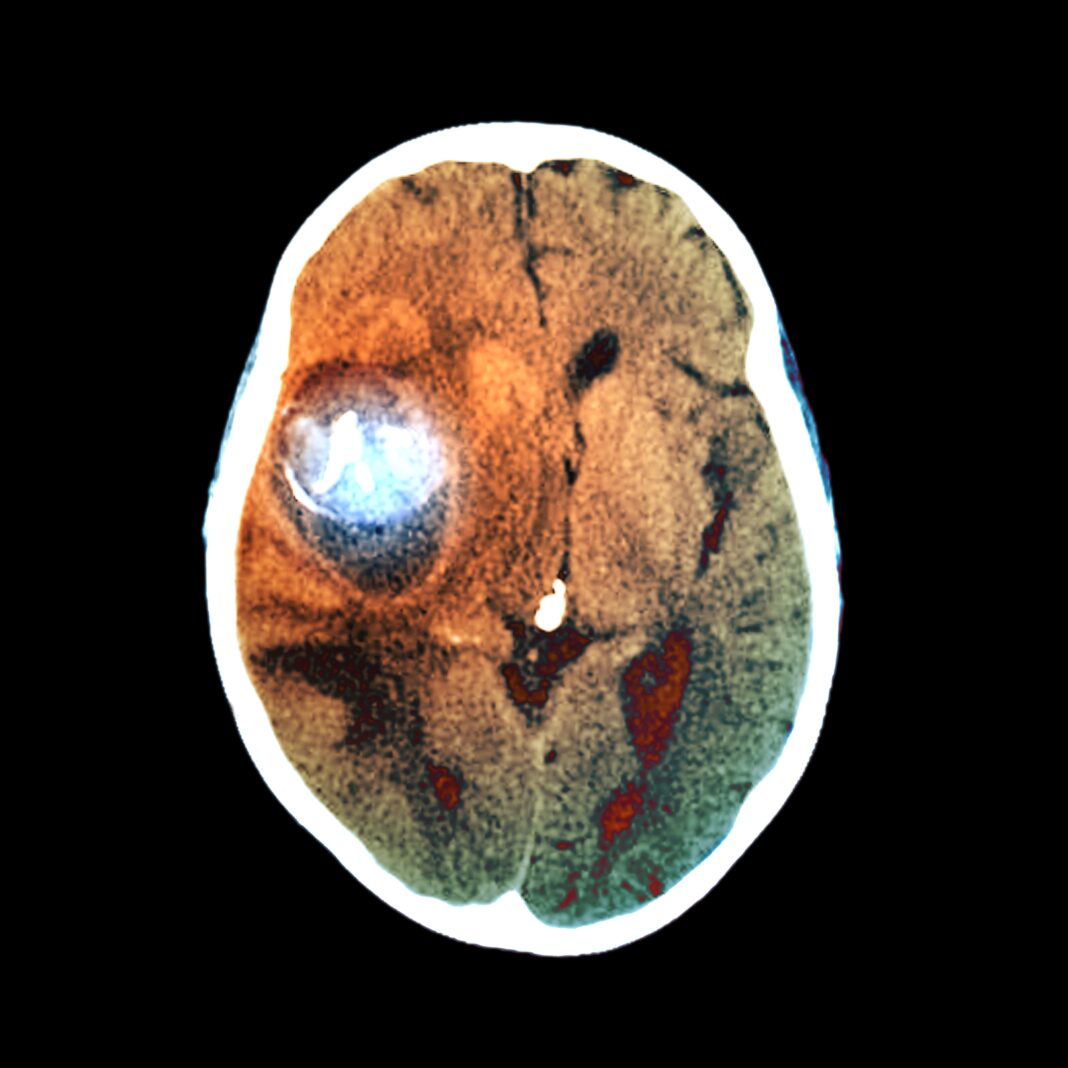
For the study, researchers looked at the records for all people with a stroke who were treated with thrombolytics at a stroke center in Finland over 15 years. After determining how many had unruptured aneurysms, they then looked to see how many people had a hemorrhagic stroke, or an intracranial hemorrhage, caused by the rupture of the aneurysm while they were in the hospital after the treatment.
Of the 3,953 people in the study, 132 people had one or more unruptured aneurysms. Of the 155 unruptured aneurysms, 141 were the type called saccular aneurysms and 14 were fusiform aneurysms. One limitation of the study was that only a small number of people had large aneurysms.
The aneurysms ruptured after treatment causing a hemorrhagic stroke in only three people, or 2.3%. All three had large aneurysms called fusiform basilar artery aneurysms. All three were treated with blood thinners after their treatment. None of the saccular type of aneurysms ruptured.
“Fortunately, today blood thinners are not commonly used early after ischemic stroke, so that may help to reduce this risk even further,” Virta said. “Our results suggest that thrombolytic therapy may be relatively safe for people with ischemic stroke even if they have larger saccular aneurysms that have not ruptured. For people with large fusiform aneurysms, additional consideration should be taken regarding treatment as blood thinners may increase the risk of aneurysm rupture.”