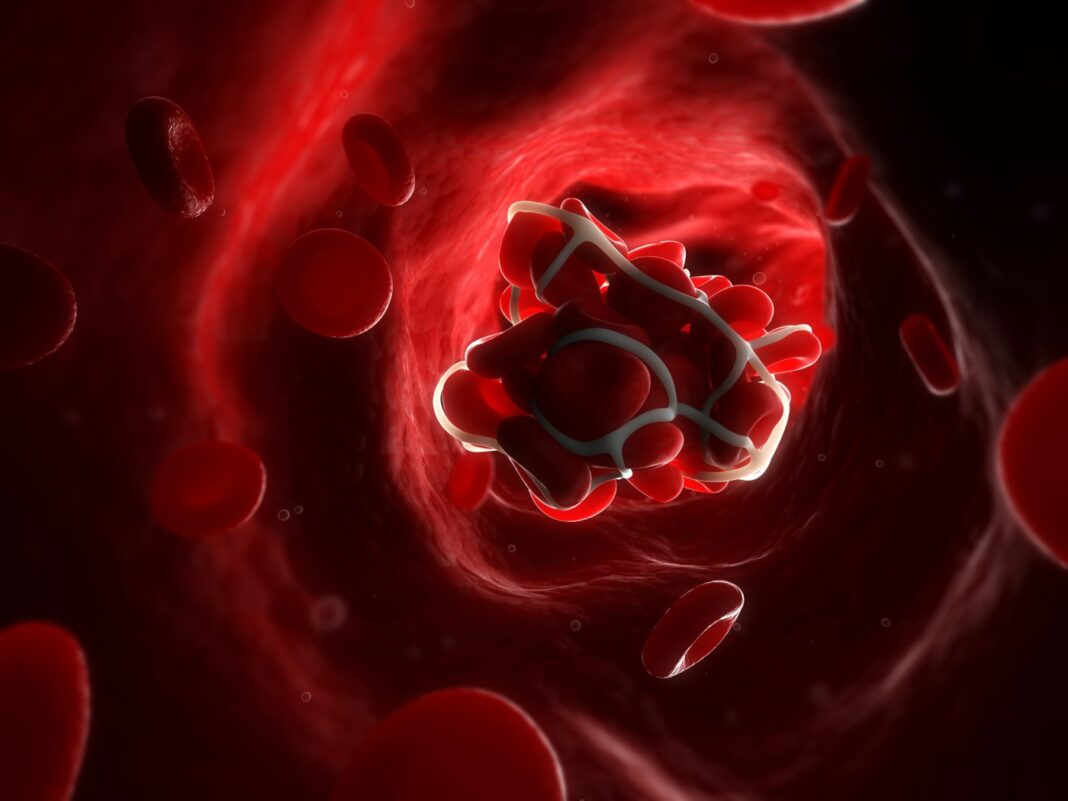
A team of researchers has uncovered how COVID-19 vaccines that use adenovirus vectors trigger a rare, but sometimes fatal, blood clotting reaction called vaccine-induced immune thrombotic thrombocytopenia (VITT). The findings will likely have both diagnostic and therapeutic implications.
The research is published in Nature in the article, “Antibody epitopes in vaccine-induced immune thrombotic thrombocytopenia.”
“The intention of our study was to better understand how the severe clots which characterize VITT develop,” said Donald Arnold, MD, chair in translational research and co-medical director of the McMaster Platelet Immunology Laboratory. “A basic principle of medical care is to understand how the disorder happens and, in doing so, develop better treatments.”
[James Smith/McMaster University]
The group first determined how platelets became activated by antibodies from patients who had VITT. They could show that VITT is caused by highly unusual antibodies to blood platelets that are triggered by the vaccine that stick to components from blood platelets causing them to trigger clot formation.
The group found that antibodies can bind tightly to a specific site on the naturally occurring platelet factor 4 (PF4) protein. Using alanine scanning mutagenesis, they studied the amino acids involved in the interaction between the VITT antibodies and PF4 protein. More specifically, they determined the binding of VITT anti-PF4 antibodies was restricted to eight surface amino acids, “all of which were located within the heparin binding site on PF4, and the binding was inhibited by heparin.”
They then used biolayer interferometry (BLI) to determine how tightly the VITT antibodies bound to the target on PF4. The authors noted that the location of binding and the strength of binding “allow the antibodies to cluster PF4 proteins together forming immune complexes that can activate platelets and trigger an intense clotting reaction throughout the body.”
“The antibodies stick to the platelet protein called platelet factor 4 (PF4) in a very unique and specific orientation, which allows them to align with other antibodies and platelets in the precise formation that leads to a self-perpetuating vicious cycle of clotting events,” said Ishac Nazy, PhD, associate professor of medicine for the Michael G. DeGroote School of Medicine at McMaster University in Ontario, Canada. “These disease-causing aggregates quickly activate platelets, creating a highly intense clotting environment in patients,” he said.
This work, Nazy added, “answers important questions about the connection between antibodies and clotting.”
John Kelton, MD, co-investigator of the study and professor of pathology and molecular medicine at McMaster, added: “We believe that this study is important because it clarifies how the clotting ensues, and because we have been able to identify the molecules involved. The next step is to develop a rapid diagnostic and accurate test to diagnose VITT. Our major interest is now to move upstream from how the clots happen to preventing them from occurring.”