Different neurons and regions in the brain are not equal when it comes to Alzheimer’s Disease. In the course of the disease’s progression, parts of the brain like the caudal entorhinal cortex are affected early on while other regions like the superior frontal gyrus are affected much later.
The cause of this “selective vulnerability” is the “million-dollar question,” says co-senior author, Lea Grinberg, MD, PhD, associate professor, department of neurology, University of California San Francisco (UCSF) Memory and Aging Center. “Imagine three people in a storm. One develops pneumonia, the other a cold, and the third, nothing. Same storm, different outcomes.”
An understanding of the molecular signatures that make a specific brain region or neuronal subtype especially vulnerable to the neurodegenerative disease would pave the way for therapeutic strategies that increase the brain’s resilience.
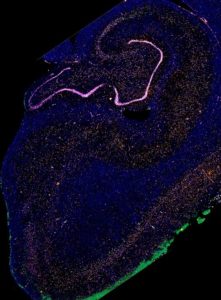
A team of molecular biologists and neuropathologists from the University of California, San Francisco Weill Institute for Neurosciences, have performed single-nucleus RNA sequencing on post-mortem brains spanning the progression of the disease to profile and compare brain regions where neurofibrillary tangles and neuronal loss occur early versus late in Alzheimer’s Disease.
“We know which neurons are first to die in other neurodegenerative diseases like Parkinson’s disease and ALS, but not Alzheimer’s,” says co-senior author, Martin Kampmann, PhD, Associate Professor, Department of Biochemistry and Biophysics, UCSF Institute for Neurodegenerative Diseases.
The authors identify RORB as a marker of vulnerable excitatory neurons in the entorhinal cortex. Using quantitative neuropathological methods, they validate the loss of RORB expressing excitatory neurons and their selective susceptibility to neurofibrillary tangles during the progression of the disease.
The authors also identify a subpopulation of astrocytes where the expression of genes involved in the normal house-keeping homeostatic functions is decreased in the post-mortem Alzheimer’s samples.
This study is reported in the article, “Molecular characterization of selectively vulnerable neurons in Alzheimer’s disease,” published in Nature Neuroscience.
Tau pathology—the production of toxic tangles of the protein tau, whose spread through the brain drives cell death and loss of memory—has long been the focus of Alzheimer’s research. But researchers have not looked closely at whether all cells are equally vulnerable to the toxic effects of these protein accumulations.
“We obtained gene expression profiles from those neurons that are vulnerable early in disease. We think that some of these differentially expressed genes are responsible for selective vulnerability. Our next step will be to use a new CRISPR-based gene perturbation technology—CRISPR Interference-Based Platform for Multimodal Genetic Screens in Human iPSC-Derived Neurons—to pinpoint which genes are causing selective vulnerability, and by what mechanisms,” says Kampmann.
RORB is a transcription factor that plays a role in the development of different neuronal subtypes by controlling a gene expression program. “Our finding suggests that some components of this gene expression program drive selective vulnerability to Alzheimer’s Disease. However, it is important to note that our study has established RORB as a marker of vulnerable neurons—future work will test whether it plays a causal role in vulnerability,” says Kampmann.
“RORB expressing neurons are found both in the entorhinal cortex and the neocortex,” says Grinberg. “Our data suggest that this type of neuron is very vulnerable to Alzheimer’s in both locations. There is no indication that the population of RORB neurons is larger in the entorhinal cortex. ROROB neurons are a relatively small population, but it turns out to be very vulnerable to Alzheimer’s.”
“By identifying that RORB neurons are more vulnerable to Alzheimer’s, we can now investigate how RORB neurons are different than other non-vulnerable neurons,” says Grinberg.
This new finding can now be harnessed to develop therapeutic strategies. “Our next goal is to pinpoint the specific factors in RORB expressing neurons that cause vulnerability. Our hope is that these factors can be targeted therapeutically to turn vulnerable neurons into resilient neurons,” says Kampmann.
“Our discovery of a molecular identifier for these selectively vulnerable cells gives us the opportunity to study in detail exactly why they succumb to tau pathology, and what could be done to make them more resilient,” says Kun Leng, first author on the study and MD/PhD student in the Kampmann lab. “This would be a totally new and much more targeted approach to developing therapies to slow or prevent the spread of Alzheimer’s disease.”
The brain tissues used in the study are obtained from the UCSF Neurodegenerative Disease Brain Bank and the Brazilian BioBank for Aging Studies, a unique resource co-founded by Grinberg. The São Paulo-based biobank collects tissue samples from a broad population of deceased individuals, including many without a neurological diagnosis whose brains nevertheless show signs of very early-stage neurodegenerative disease, which is otherwise very difficult to study in humans.



