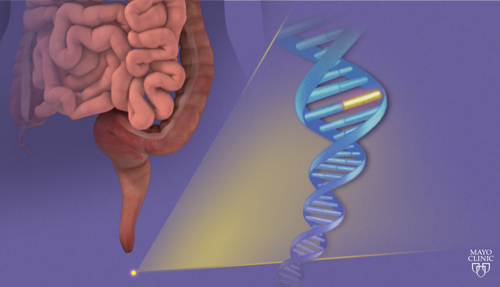
In a side-by-side comparison, a noninvasive, multitarget stool DNA test proved to be more sensitive than a fecal immunochemical test (FIT). This result, published March 19 in the New England Journal of Medicine, suggests that the DNA test, which includes quantitative molecular assays for genetic abnormalities related to cancer, could significantly improve the effectiveness of colon cancer screening.
The FIT test detects hidden blood in the stool, a potential signal for cancer. In contrast, the DNA test includes quantitative molecular assays for KRAS mutations, aberrant NDRG4 and BMP3 methylation, and β-actin, plus a hemoglobin immunoassay.
The effectiveness of the DNA test was established in a study that evaluated nearly 10,000 asymptomatic patients who were deemed to be at average risk of developing colorectal cancer. It turned out that 65 (0.7%) of these patients had colorectal cancer, and 757 (7.6%) had advanced precancerous lesions. When these patients were screened, the study determined that the sensitivity for detecting colorectal cancer was 92.3% with DNA testing and 73.8% with FIT.
The investigators who evaluated the DNA and FIT tests published their results in an article entitled “Multitarget Stool DNA Testing for Colorectal-Cancer Screening,” which indicated that “sensitivity is the most important characteristic for screening tests because the primary role of such testing is to rule out diseases such as cancer.”
Other results related to sensitivity were as follows: “The sensitivity for detecting advanced precancerous lesions was 42.4% with DNA testing and 23.8% with FIT. The rate of detection of polyps with high-grade dysplasia was 69.2% with DNA testing and 46.2% with FIT.”
The study added that although high sensitivity is the most important attribute of cancer-screening tests, specificity is also important, since it affects the number of persons who have positive test results, a majority of whom will have false-positive results because of the low prevalence of cancer: “The specificity of FIT (94.9 to 96.4%) was superior to that of the DNA test (86.6 to 89.8%), with false positive rates of 3.6 to 5.1% and 10.2 to 13.4%, respectively.”
The authors of the study represented Indiana University School of Medicine, the University of North Carolina, Icahn School of Medicine at Mount Sinai, Kaiser Permanente Medical Center, the Boston Biostatistics Research Foundation, Exact Sciences (which funded the study), and the Mayo Clinic.
One of the authors, David Ransohoff, M.D., professor of medicine at the University of North Carolina, said, “Detection of 92% of colon cancer is extremely high for a noninvasive test, so that a negative test result means that no further evaluation, like colonoscopy, is needed at that time. Having such a sensitive, noninvasive option could have an important effect on screening rates for colorectal cancer.”
The article was accompanied by an editorial entitled “Stool DNA and Colorectal-Cancer Screening.” It took note of the specificity issue and raised a couple of additional caveats: “First, the number of participants who were excluded from the study because of problems with sample collection or assay application was far greater in the stool DNA group. Given that colorectal cancer was detected in nearly 1 of 154 participants on colonoscopy, it is possible that four cancers would have been missed simply because of the complexity of the test. Second, this study compared only the one-time sensitivity of these two tests. Given the lower specificity and greater expense of stool DNA testing as compared with FIT, it is unlikely that the test would be performed annually in the way that FIT testing is recommended.”
Nonetheless, the editorial (by a pair of authors affiliated with the Veterans Administration) concluded that the “new multitarget stool DNA test is clearly an improvement over its predecessors, and the results of this study will help to inform the current effort of the U.S. Preventive Services Task Force to reevaluate screening tests.”
A press release issued by the Mayo Clinic emphasized the development of the DNA test, which is called Cologuard. “Cologuard detection rates of early-stage cancer and high-risk precancerous polyps validated in this large study were outstanding and have not been achieved by other noninvasive approaches,” said David Ahlquist, M.D., a Mayo Clinic gastroenterologist, co-inventor of the Cologuard test, and one of the study’s authors. “It is our hope that this accurate and user-friendly test will expand screening effectiveness and help curb colorectal cancer rates in much the same way as regular Pap smear screening has done for cervical cancer.”
Exact Sciences, the co-developer of Cologuard, is in the process of seeking approval from the FDA for the use of the DNA test for colorectal cancer screening. The company is scheduled to appear before the Molecular and Clinical Genetics Panel of the Medical Devices Advisory Committee on March 27.