The results of studies in mice by University of Iowa (UI) scientists suggest that the metabolism of plant-based dietary compounds by specific gut bacteria that are lacking in patients with multiple sclerosis (MS) may provide protection against the immune-mediated disease.
Research headed by Ashutosh Mangalam, PhD, UI associate professor of pathology, showed that a diet rich in plant isoflavone—a phytoestrogen that resembles estrogen—protected against MS-like symptoms in a mouse model of the disease. Importantly, the isoflavone diet was only protective when the mice had gut microbes that were capable of breaking down the isoflavones.
“Interestingly, previous human studies have demonstrated that patients with MS lack these bacteria compared to individuals without MS,” Mangalam said. “Our new study provides evidence that the combination of dietary isoflavones and these isoflavone metabolizing gut bacteria may serve as a potential treatment for MS.” The UI researchers and colleagues reported their findings in Science Advances, in a paper titled, “Isoflavone diet ameliorates experimental autoimmune encephalomyelitis through modulation of gut bacteria depleted in patients with multiple sclerosis,” in which they concluded, “Collectively, our study provides evidence that dietary-induced gut microbial changes alleviate disease severity and may contribute to MS pathogenesis.”
Multiple sclerosis is an autoimmune disease of the brain and spinal cord that results when the immune system attacks the protective myelin sheath surrounding nerve fibers. The chronic neuroinflammatory disease is caused by a complex interaction of genetic and environmental factors, which triggers the activation of autoreactive T cells, leading to immune cell infiltration into the CNS, neurodegeneration, and axonal damage, the authors explained. The symptoms of MS include muscle weakness and problems with balance, vision, and thinking. Available treatments can help to slow disease progress, but there is currently no cure for MS.
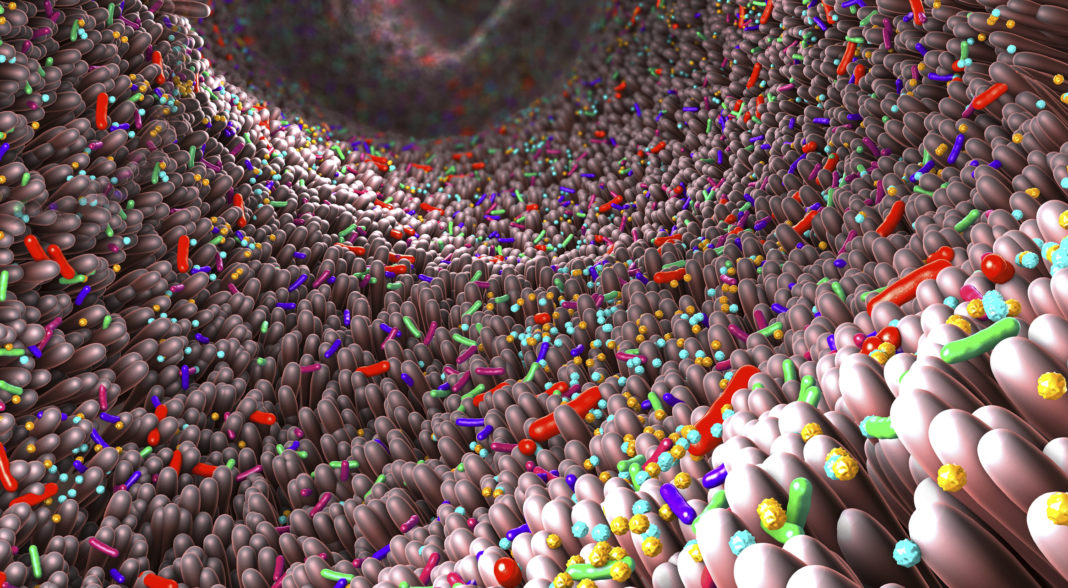
While some of the genetic influences on MS have been well characterized, the role of environmental effects, which the team said may account for some 70% of disease risk, hasn’t been so well studied. One potential environmental factor is the gut microbiome, which studies increasingly suggest influences health and disease. “Given that there are >3,000,000 genes in the gut microbiome compared to 20,000 to 25,000 protein coding genes in the entire human genome, it is expected that the gut microbiota plays a fundamental role in intestinal and systemic health,” the investigators stated. “Recently, the gut microbiome has emerged as a potential environmental factor that may ultimately provide critical clues to the pathogenesis and regulation of MS.” However, the mechanisms through which different gut bacteria might influence MS aren’t known, the team acknowledged. “Understanding the role gut microbes play in disease course may lead to possible interventions of diet, probiotics, and/or advanced combinatorial therapies for patients with MS.”
Isoflavones are a major class of phytoestrogens that are found in soybeans, peanuts, chickpeas, and other legumes. Humans don’t naturally produce the enzymes needed to break down these compounds, so we instead “… rely on the gut microbiota to harvest these biologically active metabolites,” the team stated. Interestingly, through their prior work, Mangalam and colleagues had demonstrated that there are significant differences between the gut microbes of patients with MS and people without MS. Specifically, patients with MS lacked bacteria that are able to metabolize isoflavones.
In their newly reported study, Mangalam’s team, including first author Samantha Jensen, a UI graduate student in immunology, found that the bacteria that are lacking in patients with MS are able to suppress inflammation in the experimental autoimmune encephalomyelitis (EAE) mouse model of MS. When the team then compared the effects of either an isoflavone diet or an isoflavone-free diet on disease in the animals, they found that the isoflavone diet led to disease protection. However, when EAE model mice were then placed on an isoflavone-containing diet, but their isoflavone-metabolizing gut bacteria were removed, the isoflavone diet was no longer able to protect against MS-like symptoms. When the bacteria were then reintroduced into the animals, the protective effect of the isoflavone diet was restored. “This study suggests that an isoflavone diet may be protective so long as the isoflavone metabolizing gut bacteria are present in the intestines,” said Mangalam, who also is a member of the Iowa Neuroscience institute and Holden Comprehensive Cancer Center.
The team was also able to show that a specific isoflavone metabolite called equol, which is produced by the gut bacteria from isoflavone, is able to provide protection against disease. “The disease protection and anti-inflammatory phenotype associated with an isoflavone diet that we observed relied on the presence of specific bacteria that can metabolize isoflavone into S-equol, demonstrating that isoflavone-metabolizing gut bacteria that generate isoflavone metabolites provide protection against EAE,” they wrote. “ … we found that treating mice on an isoflavone-free diet with S-equol ameliorated EAE, with disease severity similar to that of mice on an isoflavone diet.”
The study also found that mice fed the isoflavone diet had a microbiome that is similar to the microbiome found in healthy people, and which includes the isoflavone-metabolizing bacteria. Conversely, a diet lacking isoflavones promoted a microbiome in mice that is more similar to the gut microbiome observed in patients with MS, and lacks the beneficial bacteria that can metabolize isoflavone. “Notably, the composition of the gut microbiome in mice fed an isoflavone diet exhibited parallels to healthy human donors, whereas the composition in those fed an isoflavone-free diet exhibited parallels to patients with MS,” they commented. “Given that mice on an isoflavone diet can suppress EAE, these data suggest that an isoflavone diet enables the proliferation of specific gut bacteria that can improve disease outcomes in EAE and possibly MS … Collectively, these results demonstrate that the severity/development of EAE is influenced by both diet and the resulting changes in the composition of the gut microbiome.”
The authors say their results lay the groundwork for future studies investigating the cellular and molecular pathways responsible for equol-induced EAE suppression. “Ultimately, these studies will inform our use of diet and gut microbiome–based therapies as a complement to conventional disease-modifying therapies (IFN-ß, glatiramer acetate, fingolimod, ocrelizumab, etc.) for the treatment of MS and other diseases.