The appearance of SARS-CoV-2 variants has permeated the news since the beginning of the year. Viruses mutate, so new variants are not surprising. But the phenotypes associated with those changes could potentially be a cause of concern; particularly if they impact immune memory or vaccine efficacy. Now, scientists address the influence of antigenic drift (slow mutational changes over time) on immune evasion of seasonal coronaviruses. In doing so, they show that two seasonal human coronaviruses undergo adaptive evolution in regions of the viral spike protein that are exposed to human humoral immunity. The findings suggest that a continual reformulation of coronavirus vaccines may be necessary.
The work is published in eLife in the paper, “Evidence for adaptive evolution in the receptor-binding domain of seasonal coronaviruses OC43 and 229E.”
First, a quick coronavirus primer. There are hundreds of coronaviruses circulating in animals such as bats, cats, pigs, and camels. Seven coronaviruses are known to date to infect humans. The coronaviruses that commonly infect people, causing a mild infection that likely resembles the common cold, are 229E, NL63, OC43, and HKU1. The other, more notorious, group consists of MERS-CoV, SARS-CoV, and SARS-CoV-2.
“Some coronaviruses are known to reinfect humans but it is not clear to what extent this is due to our immune memory fading or antigenic drift,” said first author Kathryn Kistler, a PhD student at the Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center in Seattle. “We wanted to investigate whether there is any evidence of coronaviruses related to SARS-CoV-2 evolving to evade our immune responses.”
The research team looked at the four seasonal human coronaviruses (HCoVs). Since HCoVs have been circulating in the human population for 20–60 years, regularly infecting and reinfecting humans, it is likely that their antigens have faced pressure to evolve against the immune system.
The authors noted that it is not known to what extent reinfection by these viruses is due to waning immune memory or antigenic drift of the viruses.
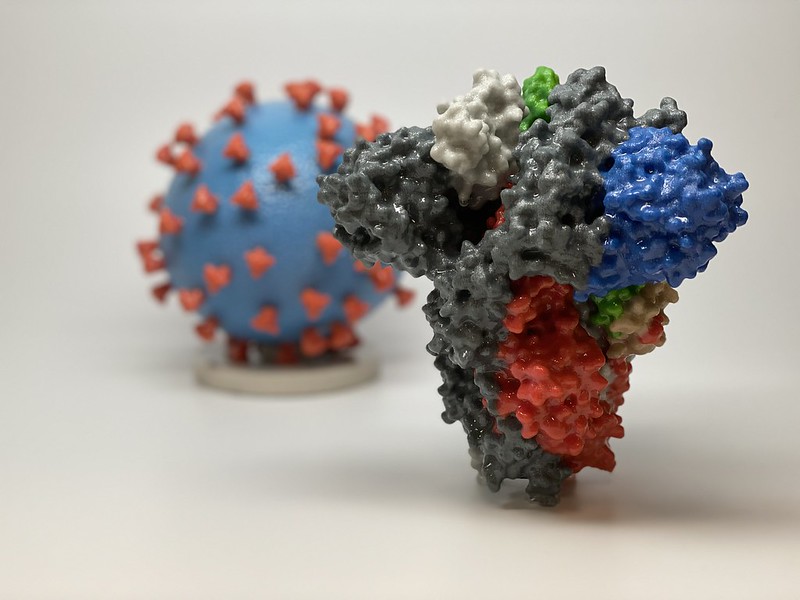
The team used a variety of computational methods to compare the genetic sequences of many different viruses, enabling them to see how they have evolved over the years. They were especially interested in any changes that might have occurred in viral proteins that could contain antigens, such as spike proteins which are on the surface of coronaviruses and are therefore exposed to the immune system.
The researchers found a high rate of evolution in the spike proteins of two of the four viruses, OC43 and 229E. Nearly all of the beneficial mutations appeared in a specific region of the spike proteins called S1, which helps the virus infect human cells. This suggests that reinfection by these two viruses can occur as a result of antigenic drift as they evolve to escape recognition by the immune system.
The team also estimated that beneficial mutations in the spike proteins of OC43 and 229E appear roughly once every two to three years, about half to one-third of the rate seen in the flu virus strain, H3N2.
“Due to the high complexity and diversity of HCoVs, it is not entirely clear if this means that other coronaviruses, such as SARS-CoV-2, will evolve in the same way,” explained Trevor Bedford, principal investigator and associate member at the Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center. “The current vaccines against COVID-19, while highly effective, may need to be reformulated to match new strains, making it vital to continually monitor the evolution of the virus’ antigens.”