Scleroderma is an autoimmune disease affecting the skin and other organs of the body. The main findings of scleroderma are thickening and tightening of the skin and inflammation and scarring of many body parts, leading to problems in the lungs, kidneys, heart, intestinal system, and other areas. Although the underlying cause is unknown, promising research is shedding light on the relationship between the immune system and scleroderma. A new study by researchers at the Weizmann Institute of Science demonstrates that fibroblasts, which have long been viewed as background players, may play a critical role in scleroderma. The findings may pave the way for future therapies against the incurable disorder.
The new study published in the journal Cell in a paper titled, “LGR5 expressing skin fibroblasts define a major cellular hub perturbed in scleroderma,” was headed by Ido Amit, PhD, professor at the Weizmann Institute of Science.
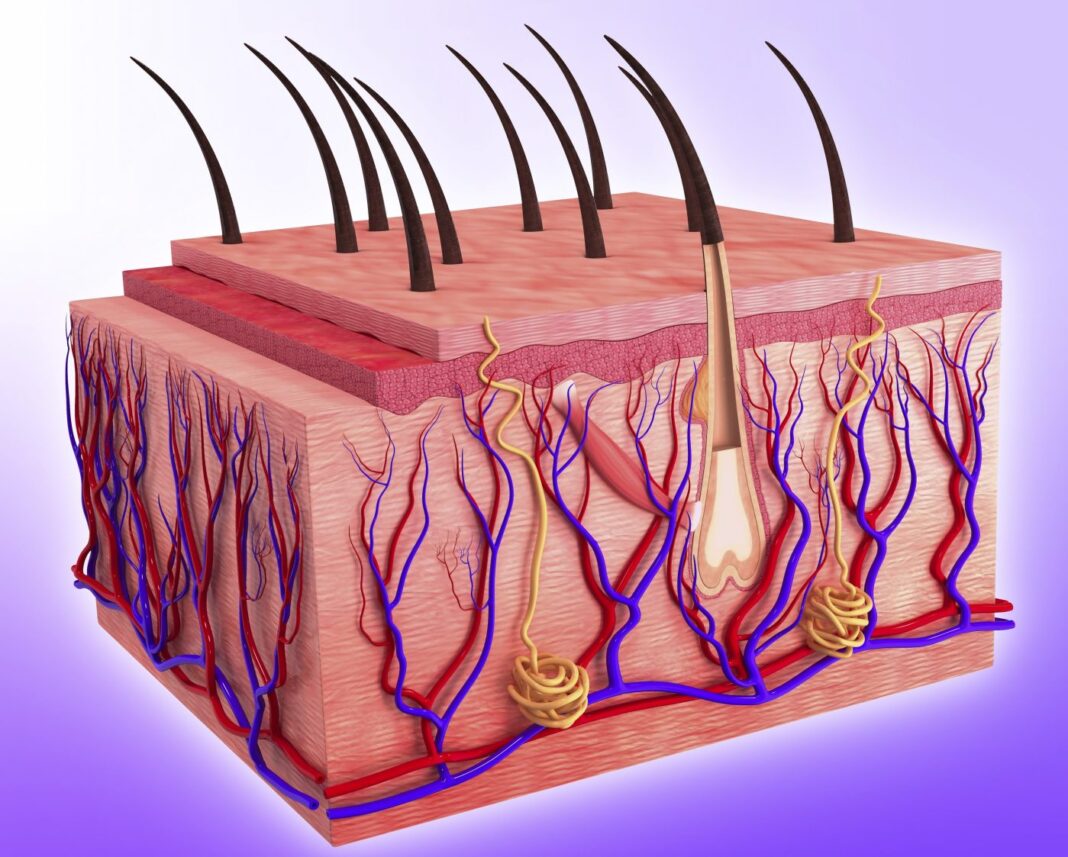
Aside from roles in growth and wound healing, fibroblasts were thought to be “scaffolding” holding cells in place.
“Systemic sclerosis (scleroderma, SSc) is an incurable autoimmune disease with high morbidity and mortality rates,” the researchers wrote. “Here, we conducted a population-scale single-cell genomic analysis of skin and blood samples of 56 healthy controls and 97 SSc patients at different stages of the disease.”
“Scleroderma is one of the most frustrating disorders to treat—we can alleviate some of the patient’s symptoms, but usually we cannot significantly affect the cause of the disease, block its progression, or reverse its course,” explained Chamutal Gur, MD, a senior physician in the rheumatology department at Hadassah University Medical Center, who led the new study in Amit’s lab in Weizmann’s immunology department.
Single-cell RNA sequencing reveals each cell’s unique identity. The researchers collected skin samples from nearly 100 scleroderma patients and from more than 50 healthy volunteers who served as a control group, in the largest-ever study of this kind to explore the disease.
The researchers managed to identify a subset of fibroblasts whose concentration drops sharply in the early stages of scleroderma. They named these cells Scleroderma-Associated Fibroblasts, or ScAFs (which is also short for “scaffold”). Whereas in healthy controls ScAFs accounted for nearly 30% of all fibroblasts, this percentage decreased dramatically in scleroderma patients and continued to plummet as the disease progressed.
The researchers mapped out the locations of ScAFs deep within skin tissue, and they tapped these cells’ RNA to determine what changes a functional ScAF into a malfunctioning cell common in scleroderma patients. They also identified biological markers correlated with specific kinds of organ damage; these markers can help physicians administer a personalized treatment, in order to prevent life-threatening complications. The research also revealed ScAF-related signaling pathways that can be targeted in future scleroderma therapies.
“The reduction in the size of a critical subset of fibroblasts appears to be an early event in the course of scleroderma,” Amit said. “It might be possible to design a therapy that will make up for this loss, slowing the progression of the disease.”
“Our approach is relevant to other diseases,” added Shuang-Yin Wang, PhD, a postdoc in Amit’s lab, who led the study’s data analysis using artificial intelligence tools. “It reveals the enormous potential of meticulous tissue analysis involving advanced single-cell technologies for uncovering disease dynamics.”
“Integrating the latest single-cell genomic research techniques with clinical data can shed new light on diseases whose origins are currently obscure,” Amit added.
“Our high-resolution atlas of the sclerodermatous skin spectrum will enable a paradigm shift in the understanding of SSc disease and facilitate the development of biomarkers and therapeutic strategies,” concluded the researchers.