The gut-brain connection is a complicated two-way signaling cascade that is responsible for keeping the digestive system working properly and can cause problems when it breaks down. In a study in mice, researchers at Harvard Medical School have now defined five distinct subtypes of sensory neurons in the colon that carry signals to the brain. Their results indicate that some neurons are dedicated to sensing gentle forces, such as substances moving through the colon, while others sense more intense ones, such as pain. The team suggests that their findings, if confirmed in humans, could help scientists develop more effective therapies to treat conditions that arise when this colon-brain sensing system goes awry.
“Patients often complain about sensation and pain in the gastrointestinal system, yet we don’t know a lot about the sensory neurons that innervate the gut and allow us to respond to different stimuli,” said Rachel Wolfson, MD, PhD, a research fellow in neurobiology at HMS and a gastroenterology fellow at Massachusetts General Hospital. Wolfson is first author of the team’s published paper in Cell, titled “DRG afferents that mediate physiologic and pathologic mechanosensation from the distal colon.”
Researchers in the lab of senior study author David Ginty, PhD, have spent many years investigating how sensory neurons in the skin communicate with the brain to form our sense of touch. The scientists have developed precise genetic tools that label subtypes of sensory neurons, and have used these tools to uncover basic information about the structure, organization, and function of skin-sensing neurons.
Yet even as scientific knowledge about touch neurons has grown, very little research has focused on understanding the neurons in other parts of the body, including the gastrointestinal system. “The properties of dorsal root ganglia (DRG) neurons that innervate the distal colon are poorly defined, hindering our understanding of their roles in normal physiology and gastrointestinal (GI) disease,” the authors wrote. “We’ve learned a lot about the neurons that go to the skin, but the properties of neurons that project to other organs like the colon have remained poorly understood,” added Ginty, the Edward R. and Anne G. Lefler Professor of Neurobiology in the Blavatnik Institute at HMS.
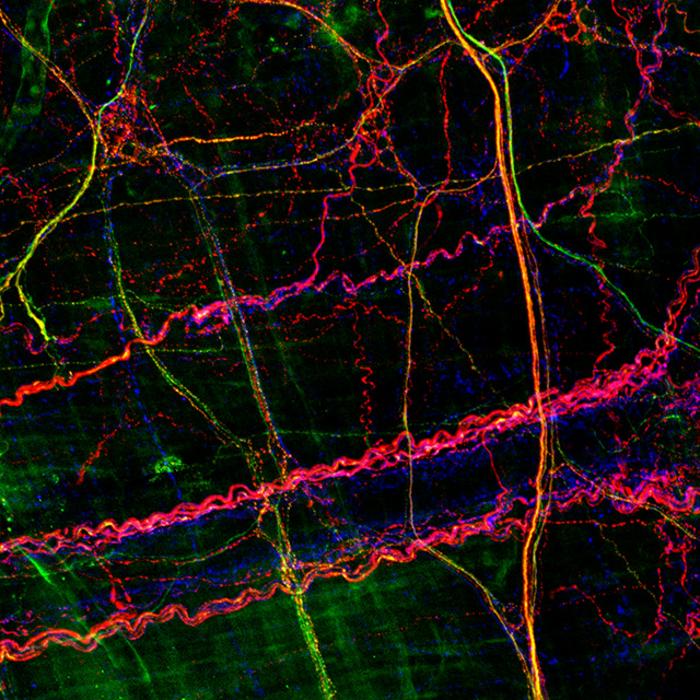
To tackle this understudied area, Ginty teamed up with Wolfson, a neurobiologist and clinical expert on the gastrointestinal system. Their study employed mouse molecular genetic approaches, morphological analyses, functional imaging, electrophysiology, and behavior to determine what they termed “the properties and functional diversity of colon-innervating DRG afferents and their roles in physiologic and pathophysiologic mechanosensation.”
For their work Wolfson took genetically labeled mouse models developed in the Ginty lab and repurposed them to study neurons in the colon. She discovered that five subtypes of sensory neurons in the skin are also found in the colon. However, colon and touch neurons had distinct shapes, and the subtypes of colon neurons also varied from each other in form.
“We know that form underlies function, so the fact that the colon neurons look different from each other made us think that they have different functions,” Wolfson said.
To investigate function, Wolfson stretched the colon with a balloon—mimicking naturally occurring distension—and recorded activity in the distinct types of neurons. Two types responded to gentle forces, similar to the slight stretching that might happen when digested food or stool moves through the colon. Two other types responded to intense forces, such as more extreme stretching. “In vivo DRG multielectrode array (MEA) recordings revealed four categories of physiologic responses to colon distension: low-threshold rapidly adapting (RA), high-threshold RA, low-threshold slowly adapting (SA), and high-threshold SA,” they explained in the paper. When Wolfson artificially activated these high-force neurons, the mice behaved as if they were in pain. When she removed the neuron with the highest force threshold, the pain response diminished. Triggering inflammation in the mice caused one of the pain-sensing neuron subtypes to become even more reactive.
Interestingly, these roles mapped onto the roles of neurons in the skin, suggesting that function may be conserved across organ systems. The study provides critical insight into the basic neurobiological mechanisms of colon sensation. “Remarkably, there is a conservation of the properties of three of the four subtypes that innervate the colon and skin,” the investigators noted. “This conservation of response properties despite distinct end organ morphologies and environments in the skin and colon implies that the genetic composition of a mechanosensory neuron type dictates its force thresholds and adaptions to sustained stimuli.”
Ginty added, “For the first time, we’ve been able to figure out the anatomy, physiology, and functions of neurons that innervate the colon.” In the short term, the researchers want to understand why colon neurons look different from their skin counterparts, and how these differences in form translate into differences in the way they behave.
“This finding is really provocative and provides a whole other direction for the work around understanding how the neurons convert mechanical forces into electrical signals, which is the currency of the nervous system,” Ginty said.
In the longer term, Wolfson plans to study the neurons in other parts of the gastrointestinal tract. She also wants to explore how colon neurons respond to other stimuli such as toxins or a lack of blood flow, which can cause abdominal pain. While the results would first have to be confirmed in humans, the researchers say their work could one day inform the development of better therapies for various gastrointestinal conditions.
“We’ve known about the innervation of the gut for 100 years, but modern neuroscience tools allow us to dig in and understand how it all works, and that’s going to serve as a platform for therapeutic approaches to treating colon problems,” Ginty said.
Targeting low-force neurons could be helpful for treating motility-related conditions like constipation and diarrhea, while targeting high-force neurons could be useful for treating pain that originates in the colon. Of particular interest is the neuron subtype that is sensitive to inflammation, which is a source of pain for patients with inflammatory bowel disease.
“Having a way to target these neurons to treat a patient’s pain while we’re getting the inflammation under control with anti-inflammatory medications is a huge therapeutic need,” Wolfson said. Noting limitations of their study, the authors nevertheless concluded “Thus, like cutaneous DRG mechanoreceptor populations, colon-innervating mechanoreceptors exhibit distinct anatomical and physiological properties and tile force threshold space, and genetically defined colon-innervating HTMRs [high threshold mechanoreceptors] mediate pathophysiological responses to colon distension, revealing a target population for therapeutic intervention.”