The monoclonal antibodies made by the New York-based company Regeneron, designed to target SARS-CoV-2, are currently the most talked about antibodies in the world. Not only because they are a lead COVID-19 drug candidate, but also because they were the first treatment that President Trump received upon receiving his COVID-19 diagnosis.
Now, a new report evaluates the in vivo efficacy of this antibody cocktail in both rhesus macaques and golden hamsters, which may model more severe disease. The study demonstrates that REGN-COV-2 can greatly reduce virus load in lower and upper airways and decrease virus-induced pathological sequelae when administered prophylactically or therapeutically in rhesus macaques. Similarly, administration in hamsters limited weight loss and decreased lung titers and evidence of pneumonia in the lungs.
The work is published in Science in the paper titled, “REGN-COV2 antibodies prevent and treat SARS-CoV-2 infection in rhesus macaques and hamsters.”
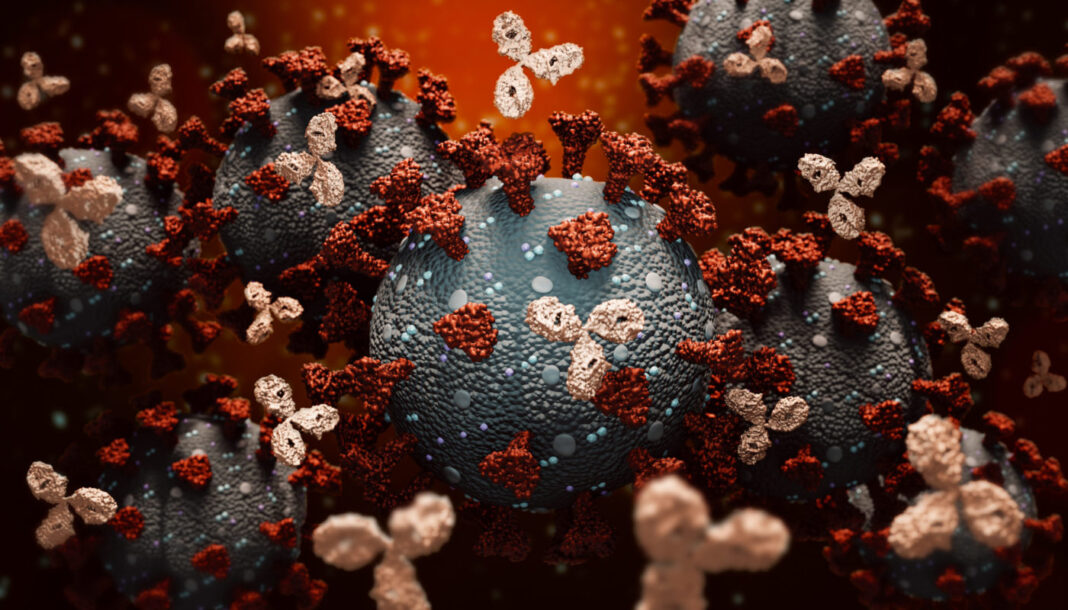
The antibodies, known as REGN-COV2, are a cocktail of two potent neutralizing antibodies (REGN10987+REGN10933) targeting non-overlapping epitopes on the SARS-CoV-2 spike protein. The cocktail began its first clinical trial in June, a month later advanced to Phase III, and is now under study in four late-stage clinical trials estimated to recruit at least a combined 11,074 participants.
In June, two studies in Science reported an antibody cocktail against SARS-CoV-2 developed from studies in humanized mice and recovering patients. Now, expanding upon this work, researchers show this antibody cocktail offers benefits in animal models that mimic the diverse pathology of SARS-CoV-2 infection, both when administered prophylactically and therapeutically.
“These findings highlight the therapeutic potential of [this approach] to both protect from and treat SARS-CoV-2 disease,” the authors wrote.
How were the antibodies tested? Six monkeys were given REGN-COV2 (mAb) and six were given placebo, through intravenous administration. They were then challenged with virus through intranasal and intratracheal routes three days after being dosed with antibodies.
To determine the impact of mAb prophylaxis on viral load in upper and lower airways, the researchers collected nasopharyngeal swabs on a daily basis and bronchoalveolar lavage (BAL) fluid on days 1, 3, and 5 post-challenge. They then measured both genomic RNA and subgenomic RNA (which is made during replication) to assess the impact of the antibodies on the dynamics of viral replication. The authors noted that while genomic RNA (gRNA) may reflect remaining viral inoculum as well as newly replicating virus, subgenomic RNA (sgRNA) should only result from newly replicating virus.
The authors wrote that, for animals receiving REGN-COV2 prophylaxis, “accelerated clearance of gRNA with almost complete ablation of sgRNA in the majority of the animals was observed, showing that REGN-COV2 can almost completely block establishment of virus infection.”
The result was seen across all measurements in both nasopharyngeal swabs and BAL compared to placebo animals, demonstrating that mAbs administered prophylactically can greatly reduce viral load in both upper and lower airways.
While multiple studies have described discovery and characterization of potent neutralizing monoclonal antibodies against SARS-CoV-2, evaluation of the efficacy of these antibodies in vivo is limited, and it’s largely focused on the prophylactic setting. As well, no single animal model has emerged as being more relevant for human disease, which has led some to say multiple animal models may be required to mimic various settings of human infection.
When administered three days before viral challenge, treatment almost completely blocked establishment of viral infection in macaques, the authors wrote. This ability, they noted, “matches or exceeds the effects recently shown in vaccine efficacy studies using the same animal models.”
In macaques treated with the drug one day after infection, the authors reported faster viral clearance than in controls who’d not been treated. Next, the authors used the hamster model to evaluate the drug’s ability to alter the disease course in more severe cases. Hamsters treated with the drug two days before infection exhibited “dramatic protection from weight loss” and decreased viral load in the lungs, the authors wrote. They also reported benefits for hamsters treated one day after infection, as compared to controls.
Taken together the two hamster studies suggest that REGN-COV2 can alter the course of infection in the hamster model of SARS-COV-2 either when administered prophylactically or therapeutically.
There were no signs of increased viral load or worsening of pathology in the presence of antibodies at either high or low doses in either animal model, which is important to note as the potential for antibody-mediated enhancement of disease (ADE) is a serious concern for antibody-based therapeutics and vaccines.
“In conclusion,” said the authors, “our data provide evidence that REGN-COV2 based therapy may offer clinical benefit in both prevention and treatment settings of COVID-19 disease, where it is currently being evaluated.”