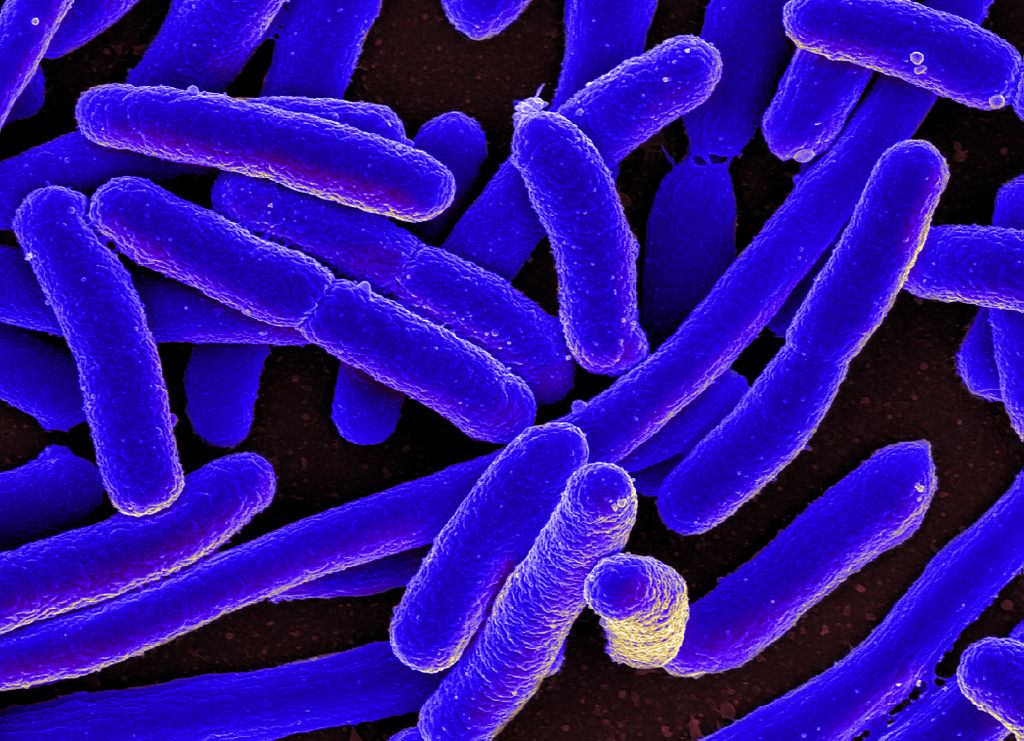
The antibiotic resistance crisis is worsening due to an increase in both the number of infections and the number of resistant strains of bacteria. A new cluster of four liver transplant recipients has been identified in New York City that carry E. coli with the rare antibiotic resistance gene mcr-1.
“Our findings were part of a prospective surveillance study of patients with a weakened immune system, and our characterization of these isolates had originally missed this type of resistance, since it is not identified by conventional drug susceptibility testing,” said principal investigator Anne-Catrin Uhlemann, MD, PhD, associate professor, Columbia University Vagelos College of Physicians and Surgeons. “While mcr-1 has been described from other parts of the world, it has been very rare in the U.S.”
The report of the detection of mcr-1-carrying E. coli ST117 was published in a paper titled, “Escherichia coli harboring mcr-1 in a cluster of liver transplant recipients: detection through active surveillance and whole genome sequencing” in Antimicrobial Agents and Chemotherapy, a journal of the American Society for Microbiology.
Mcr-1, a plasmid-associated gene for colistin resistance, is a type of polymyxin that is an antibiotic of “last resort” against some multi-drug resistant Gram-negative bacterial (MDR-GNB) infections.
The gene was first described in China in 2015 with widespread dissemination noted, but only 53 U.S. cases have been reported to date. Using whole genome sequencing, the investigators found that the bacteria in each patient, while closely related to each other, were not identical. “We then reviewed the clinical course of each individual and noted that the first patient had presented with an infection, whereas the other three only carried the bacteria in their feces,” said Uhlemann. “None of these three patients developed an infection with these bacteria.”
Because three patients showed no symptoms, the risk of spread is raised. “The detection of this cluster demonstrates the potential for silent dissemination of mcr-1 in the U.S. hospital setting, through asymptomatic colonization,” said Uhlemann. However, Uhlemann emphasized that the team’s molecular survey of more than 500 samples detected no additional cases, and that “colonization was not associated with clinical infection.”
“We routinely examine the stool samples from patients undergoing liver transplantation for colonization with drug-resistant bacteria,” said Uhlemann. “Although we documented acquisition of mcr-1 colonization in several liver transplant recipients through active surveillance of fecal MDR-GNB carriage and WGS, this is a highly resource intensive approach and is not applicable on a larger scale. A more viable alternative may be to implement PCR screening of discarded specimens (e.g., stool samples or rectal swabs),” the authors wrote.
“These findings highlight the need for ongoing surveillance of mcr-1 and other forms of transferrable resistance to polymyxins in the U.S.,” the authors added. They further suggest that patients with a weakened immune system are at particular risk to acquire these types of bacteria, and are important to study. In order to stop further spread of emerging forms of polymyxin resistance, further surveillance approaches need to recognize that clinical isolates may only represent the tip of the iceberg formed by the burden of asymptomatic colonization.