Although there is much attention being directed toward SARS-CoV-2, the coronavirus at the center of the global pandemic, there are multiple coronaviruses that infect humans. These seasonal coronavirus infections occur frequently and typically result in a mild, common cold-like illness. The presence of these coronavirus infections in the population has led to the hypothesis that immune cross-reactivity among these related viruses could occur, and potentially offer some protection to SARS-CoV-2. Now, a group of scientists has detected preexisting antibody-driven immunity against SARS-CoV-2 in a small proportion of individuals who were uninfected at the time of sampling.
This work is published in Science in the paper, “Preexisting and de novo humoral immunity to SARS-CoV-2 in humans.”
The four coronaviruses that result in a common cold-like infection when infecting humans are 229E (alpha coronavirus), NL63 (alpha coronavirus), OC43 (beta coronavirus), and HKU1 (beta coronavirus). The other three coronaviruses known to infect humans cause far more serious infections. They are MERS-CoV (the beta coronavirus that causes Middle East Respiratory Syndrome, or MERS), SARS-CoV (the beta coronavirus that causes SARS), and SARS-CoV-2, the novel coronavirus that causes COVID-19.
People around the world commonly get infected with human coronaviruses 229E, NL63, OC43, and HKU1.
The London-based group of researchers found that 16 out of 302 adults (5.3%) harbored IgG antibodies that were likely generated during previous seasonal “common cold” coronavirus infections, and which cross-reacted with subunit S2 of the SARS-CoV-2 spike protein complex.
Notably, the presence of these cross-reactive IgG antibodies was much more prevalent in an additional cohort of SARS-CoV-2-uninfected children and adolescents (aged 1 to 16 years): at least 21 of these 48 subjects (43.8%) had detectable levels of SARS-CoV-2 S-reactive IgG antibodies.
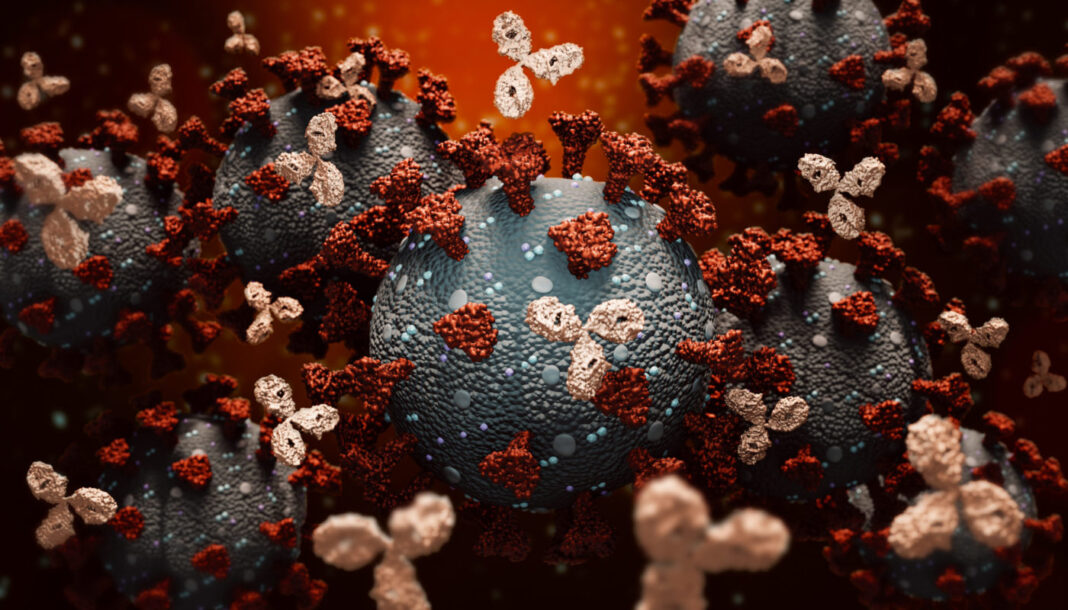
Using flow cytometry, Kevin Ng, a graduate student at the Francis Crick Institute, and colleagues, found that the SARS-CoV-2-reactive antibodies from uninfected individuals were predominantly of the IgG class—rather than IgM or IgA antibodies—that targeted the viral S2 protein, responsible for cell entry and thought to more similarly structured across different coronaviruses than subunit S1.
By contrast, the authors wrote, “SARS-CoV-2 infection induced higher titers of SARS-CoV-2 S-reactive IgG antibodies, targeting both the S1 and S2 subunits, and concomitant IgM and IgA antibodies, lasting throughout the observation period.” Notably, they continued, “SARS-CoV-2-uninfected donor sera exhibited specific neutralizing activity against SARS-CoV-2 and SARS-CoV-2 S pseudotypes.”
In cell culture experiments, sera from both older and younger uninfected individuals with cross-reactive antibodies showed the ability to neutralize SARS-CoV-2 and SARS-CoV-2 S pseudotypes, whereas sera from uninfected patients lacking cross-reactive antibodies exhibited no such neutralizing activity. Further exploring potential targets on S2 that are conserved across multiple coronaviruses may hold the promise of a universal coronavirus vaccine, the authors said.
Together, these findings may help explain higher COVID-19 susceptibility in older people and provide insight into whether pre-established immunity to seasonal coronaviruses offers protection against SARS-CoV-2.
Though previous studies suggest cross-reactive immunity is neither sterilizing nor long-lasting, the presence of cross-reactivity can reduce viral transmission and ameliorate symptoms and is, therefore, an important area of study. The authors noted that distinguishing preexisting and de novo immunity “will be critical for our understanding of susceptibility to and the natural course of SARS-CoV-2 infection.”