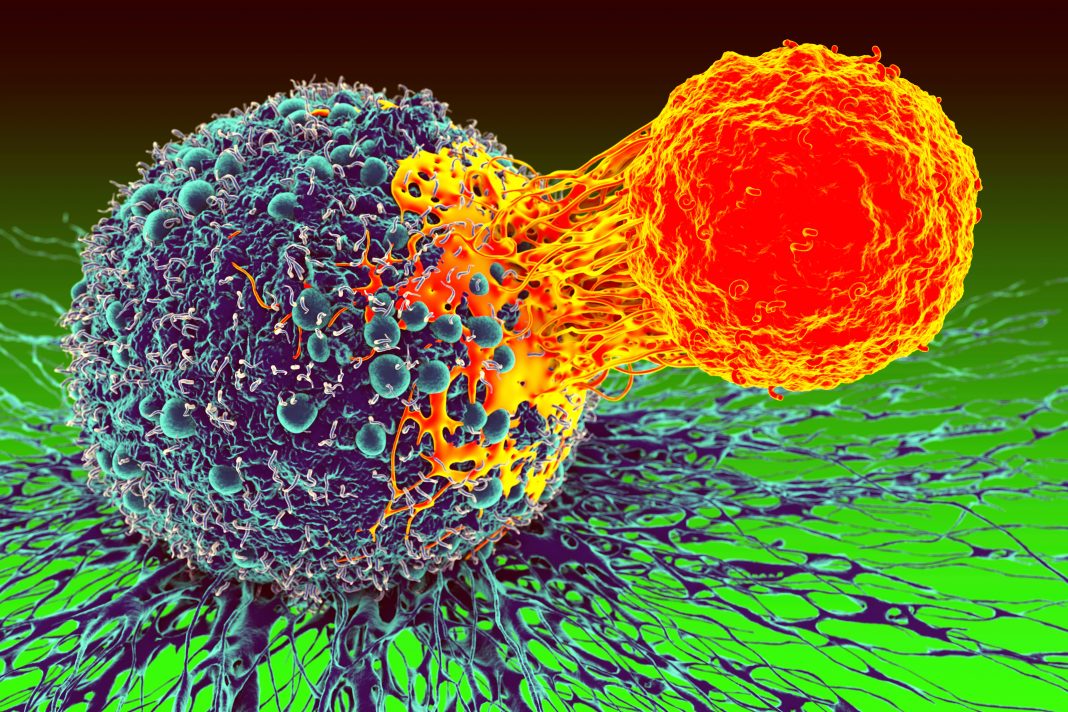
A research team led by UCLA Jonsson Comprehensive Cancer Center scientists has identified and analyzed the steps by which immune cells “see” and respond to cancer cells. Their findings may lead to more personalized immunotherapies for patients whose immune systems do not appear to respond to treatment.
The study is published in Nature in a paper titled, “Neoantigen-targeted CD8+ T cell responses with PD-1 blockade therapy.”
“Neoantigens are peptides derived from non-synonymous mutations presented by human leukocyte antigens (HLAs), which are recognized by antitumor T cells,” the researchers wrote. “The large HLA allele diversity and limiting clinical samples have restricted the study of the landscape of neoantigen-targeted T cell responses in patients over their treatment course. Here we applied recently developed technologies to capture neoantigen-specific T cells from blood and tumors from patients with metastatic melanoma with or without response to anti-programmed death receptor 1 (PD-1) immunotherapy. We generated personalized libraries of neoantigen–HLA capture reagents to single-cell isolate the T cells and clone their T-cell receptors (neoTCRs).”
“This is an important step forward in our understanding of what the T-cell responses see in the tumor and how they change over time while they are in the tumor and in circulation in the blood, searching for new tumor cells to attack,” explained Cristina Puig-Saus, PhD, a UCLA Jonsson Comprehensive Cancer Center researcher, adjunct assistant professor of medicine at UCLA, and the first author of the study.
“The deeper understanding of how the T-cell responses clear metastatic tumor masses will help us design better treatments and engineer T cells in multiple ways to mimic them,” she said.
The researchers adapted advanced gene-editing technology to make observations about immune responses in patients with metastatic melanoma receiving anti-PD-1 “checkpoint inhibitor” immunotherapy.
“With this work, we can know exactly what the immune system of a particular patient recognized in their cancer to differentiate it from normal cells and attack it,” said Antoni Ribas, MD, PhD, a UCLA Jonsson Comprehensive Cancer Center researcher, professor of medicine at UCLA, and a co-senior author of the study.
“This study demonstrates that patients without response to therapy still induce a tumor-reactive T-cell response,” Puig-Saus said. “These T cells could potentially be isolated and their immune receptors used to genetically modify a larger number of T cells to redirect them against the patient’s tumor. These T cells could be expanded in culture and reinfused into the patients to treat their tumors.”
Of the 11 patients studied, seven had a response to PD-1 blockade; four did not. The number of mutations in the tumors ranged between 3,507 and 31. In patients with clinical benefit from the therapy, the responses were diverse, with a range between 61 and seven different mutation-specific T cells isolated in the blood and the tumor. In contrast, in the patients lacking a response to therapy, the researchers only identified between 14 and two different T cells.
The study showed that immune receptors from the T cells isolated from all patients—regardless of response or not—redirected the specificity of immune cells against the tumor, producing antitumor activity.
“With this technique, we generated large numbers of T cells expressing the immune receptors from the mutation-reactive T cells isolated from each patient. We used these cells to characterize the reactivity of the immune receptors against the patient’s own cancer cells,” Ribas said. “The new technologies allow us to study these rare immune cells that are the mediators of immune responses to cancer.”