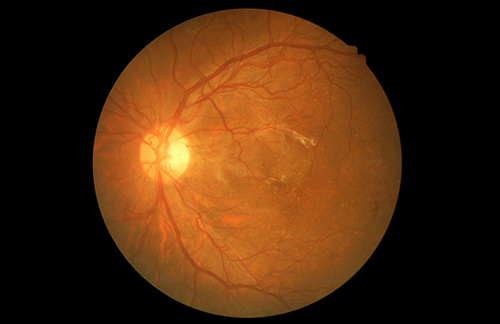
Diabetic retinopathy is one of the main vascular complications of type 2 diabetes, and the most common cause of visual deterioration in adults. A new study “The Anti-Inflammatory Effects of Glucagon-Like Peptide Receptor Agonist Lixisenatide on the Retinal Nuclear and Nerve Fiber Layers in an Animal Model of Early Type 2 Diabetes” in The American Journal of Pathology, published by Elsevier, reports on the efficacy of a possible treatment candidate that showed anti-inflammatory and neuroprotective effects on the retina and optic nerve head in early type 2 diabetic retinopathy using a diabetic mouse model.
Although the cause of diabetic retinopathy is usually attributed to hyperglycemia, several studies have shown that inflammation is also an important factor in the progression of the disorder.
“Inflammation causes neurodegeneration as well as microvascular abnormalities in the retina,” explained lead investigator Jin A. Choi, PhD, Department of Ophthalmology and Visual Science, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea. “Diabetic retinal neurodegeneration can occur before the onset of clinical diabetic retinal microvascular abnormalities. Therefore, therapeutics for neurodegeneration may provide a novel interventional strategy in the window period between the diagnosis of type 2 diabetes and the onset of clinically manifested diabetic retinopathy.”
“ This study explored the anti-inflammatory effects of a glucagon-like peptide-1 receptor agonist (GLP-1RA), known as lixisenatide, on the eyes of early type 2 diabetic mice. Diabetic (db/db) mice were divided into three groups: GLP-1RA [lixisenatide (LIX)], insulin (INS) with controlled hyperglycemia based on the glucose concentration of lixisenatide, and diabetic control (D-CON). Nondiabetic control mice (db/dm) were also characterized for comparison. After 8 weeks of treatment, mRNA levels of inflammatory markers, terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling, immunohistochemical staining; Western blot of glial fibrillary acidic protein (GFAP) and thioredoxin-interacting protein; and retinal thickness were assessed in the central and peripheral neurosensory retina,” write the investigators.
“LIX showed decreased immunohistochemical staining for both thioredoxin-interacting protein and GFAP in the central and peripheral neurosensory retina compared with D-CON and INS, and decreased expression of these proteins in the neurosensory retina and immunohistochemical staining in the optic nerve head for GFAP compared with D-CON. The inner nuclear layer in the peripheral retina in LIX was only thinner than those of D-CON and INS. In an early type 2 diabetic mouse model, lixisenatide treatment showed superior anti-inflammatory effects on the retina and optic nerve head independent of hyperglycemia.”
“Thus, the neuroprotective effects of lixisenatide treatment in the peripheral inner nuclear layer should be evaluated in early type 2 diabetic retinopathy.”
The scientists analyzed and compared the anti-inflammatory and neuroprotective effects of the glucagon-like peptide-1 receptor agonist (GLP-1RA) lixisenatide in the retina and the optic nerve head with those of insulin in a mouse model of type 2 diabetes. They divided diabetic mice into three groups; GLP-1RA (LIX); insulin (INS) with controlled hyperglycemia based on the glucose concentration of LIX; and a control group (D-CON). Nondiabetic control mice were also characterized for comparison.
After eight weeks of treatment, neuroinflammation caused by type 2 diabetes was significantly reduced in GLP-1RA-treated retinas and optic nerve heads compared with untreated or even insulin-treated retinas of early type 2 diabetic mice, showing that the outcomes are independent of the glucose-lowering effect of GLP-1RA.
“This study can provide a possible therapeutic strategy to prevent visual deterioration by using GLP-1RA in early type 2 diabetic retinopathy,” noted first author Yeon Woong Chung, MD, Choi’s colleague. “GLP-1RA significantly suppressed neuroinflammation in the early diabetic retinopathy, whereas insulin had little or no suppressive effect in this study.”
“Retinal ganglion cells start to die even before clinical changes such as hemorrhages in diabetic retinopathy occur,” commented Choi. “Thus, for better visual prognosis, we need to focus on the treatment of the retina in early type 2 diabetes before the clinical onset of diabetic retinopathy. The diabetic mouse group in our study who were treated with GLP-1RA showed significantly decreased cell death compared to those with insulin treatment.”