As a large portion of society continues to advance into age groups that are at the highest risk for the onset of neurodegenerative diseases, it has become increasingly important to gain a greater understanding of the underlying mechanisms that mediate the onset and progression of these illnesses. A growing body of evidence has linked mitochondrial dysfunction to some of the most devastating forms of neurodegeneration, such as Parkinson’s disease, different ataxias, and several peripheral neuropathies. However, despite the urge to find strategies to prevent or arrest neurodegeneration, our understanding of the precise events underlying neuronal death caused by mitochondrial dysfunction is very limited.
“We generally tend to consider neurons as terminally differentiated cells with very limited or no capacity to adapt their energy metabolism to challenging conditions,” explained lead study investigator Elisa Motori, PhD, a guest scientist at the Max Planck Institute for Biology of Aging. “For some neurological diseases, there is ample evidence that mitochondrial dysfunction can be tolerated for lengthy periods of time. We, therefore, asked the question of whether degenerating neurons may activate a program of metabolic resilience.”
Now, in a new study, researchers from the Max Planck Institute for Biology of Aging in Cologne, Germany, and the Karolinska Institute in Stockholm, Sweden, challenge the central dogma about mitochondria by showing that neurons have the potential to counteract degeneration and promote survival by adapting their metabolism. Findings from the new study were published recently in Science Advances through an article titled “Neuronal metabolic rewiring promotes resilience to neurodegeneration caused by mitochondrial dysfunction.”
As the power plants of our cells, mitochondria play an essential role in providing energy for the normal function of the tissues in our body. Nerve cells are particularly dependent on mitochondria for their activity and decreased mitochondrial function is seen in both inherited and more common age-associated forms of degenerative diseases. A long-standing view has been that neurons, in contrast to other cell types, cannot adjust their metabolism to compensate for mitochondrial dysfunction, and therefore irreversibly degenerate.
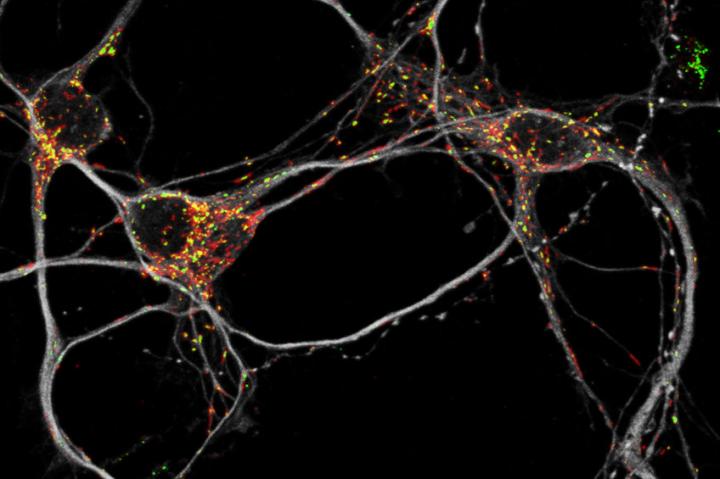
In the current study, the researchers devised an innovative approach to purify degenerating neurons from the mouse brain and analyze the global protein content (proteome) of these neurons. “Unexpectedly, the proteomic data showed the existence of a precisely coordinated, neuron-specific metabolic program that becomes activated in response to mitochondrial dysfunction,” Motori added.
“We profiled the cell-specific proteome of Purkinje neurons undergoing progressive OXPHOS deficiency caused by disrupted mitochondrial fusion dynamics,” the authors wrote. “We found that mitochondrial dysfunction triggers a profound rewiring of the proteomic landscape, culminating in the sequential activation of precise metabolic programs preceding cell death. Unexpectedly, we identified a marked induction of pyruvate carboxylase (PCx) and other anaplerotic enzymes involved in replenishing tricarboxylic acid cycle intermediates. Suppression of PCx aggravated oxidative stress and neurodegeneration, showing that anaplerosis is protective in OXPHOS-deficient neurons. Restoration of mitochondrial fusion in end-stage degenerating neurons fully reversed these metabolic hallmarks, thereby preventing cell death.”
In particular, the authors identified a form of metabolic rewiring (Krebs cycle anaplerosis) that makes neurons resistant to an otherwise very rapidly progressing degeneration. This type of metabolic adaptation was previously only thought to occur in peripheral tissues or supporting cells (glial cells) in the brain.
“The finding that neurons can induce anaplerosis was not only intriguing, but we could further demonstrate that it had a protective role. When we blocked anaplerosis, neurons died at a much faster pace, and the disease became more severe,” Motori stated.
The identification of certain forms of metabolic rewiring in dysfunctional neurons provides new mechanistic insights into the processes leading to neurodegeneration. Based on these new findings, the authors hope that it may be possible to develop therapeutic approaches to prolong neuronal survival and improve function in patients with mitochondrial diseases and other types of neurodegeneration.
“Our findings identify a previously unappreciated pathway conferring resilience to mitochondrial dysfunction and show that neurodegeneration can be reversed even at advanced disease stages,” the authors concluded.