Islet transplantation has emerged over the past few decades as a potential cure for type 1 diabetes. However, transplantation efforts have faced setbacks as the immune system continues to eventually reject new islets. Current immunosuppressive drugs offer inadequate protection for transplanted cells and tissues and are plagued by undesirable side effects.
Now, a team of researchers has discovered a technique to make immunomodulation more effective using nanocarriers to re-engineer the commonly used immunosuppressant rapamycin. Using their rapamycin-loaded nanocarriers, the researchers generated immunosuppression capable of targeting specific cells related to the transplant without suppressing wider immune responses.
The findings were published in Nature Nanotechnology, in the paper titled, “Subcutaneous nanotherapy repurposes the immunosuppressive mechanism of rapamycin to enhance allogeneic islet graft viability.”
Rapamycin is commonly used to suppress immune responses during various treatments and transplants, notable for its wide range of effects on many cell types throughout the body. However, the authors noted that standard oral rapamycin (Rapamune) administration is plagued by poor bioavailability and broad biodistribution.
“To avoid the broad effects of rapamycin during treatment, the drug is typically given at low dosages and via specific routes of administration, mainly orally,” said Evan Scott, PhD, associate professor of biomedical engineering at Northwestern’s McCormick School of Engineering. “But in the case of a transplant, you have to give enough rapamycin to systemically suppress T cells, which can have significant side effects like hair loss, mouth sores, and an overall weakened immune system.”
“We wondered, can rapamycin be re-engineered to avoid nonspecific suppression of T cells and instead stimulate a tolerogenic pathway by delivering the drug to different types of immune cells?” Scott said. “By changing the cell types that are targeted, we actually changed the way that immunosuppression was achieved.”
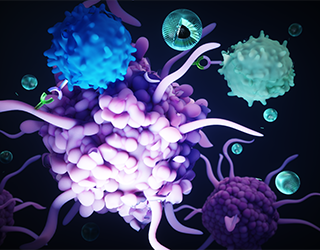
The team formulated the poly(ethylene glycol)-b-poly(propylene sulfide) polymersome nanocarrier and drug mixture to have a more specific effect than T-cell suppression. Instead of directly modulating T cells—the most common therapeutic target of rapamycin— the nanoparticle was designed to target and modify antigen-presenting cells (APCs) that allow for more targeted, controlled immunosuppression.
The nanocarrier enabled the team to deliver rapamycin through a subcutaneous injection, which uses a different metabolic pathway to avoid extensive drug loss that occurs in the liver following oral administration.
The work demonstrated that subcutaneous delivery via nanocarriers, “significantly alters rapamycin’s cellular biodistribution to repurpose its mechanism of action for tolerance, instead of immunosuppression, and minimize side effects.” In addition, the route of administration requires significantly less rapamycin to be effective—about half the standard dose.
Testing in mice, the standard Rapamune oral regimen was compared to the nanocarrier formulation. The team observed, “significantly improving maintenance of normoglycemia in a clinically relevant, major histocompatibility complex-mismatched, allogeneic, intraportal (liver) islet transplantation model.”
The concept of enhancing and controlling side effects of drugs via nanodelivery is not a new one, Scott said. “But here we’re not enhancing an effect, we are changing it—by repurposing the biochemical pathway of a drug, in this case, mTOR inhibition by rapamycin, we are generating a totally different cellular response.”

Burke, who was diagnosed with type 1 diabetes when she was nine, knew that she wanted to contribute to the field. “At my past program, I worked on wound healing for diabetic foot ulcers, which are a complication of type 1 diabetes,” Burke said. “As someone who’s 26, I never really want to get there, so I felt like a better strategy would be to focus on how we can treat diabetes now in a more succinct way that mimics the natural occurrences of the pancreas in a non-diabetic person.”
Scott has begun the process of patenting the method and collaborating with industry partners to ultimately move it into the clinical trials stage. Commercializing this work may address some issues that have arisen for new technologies like Vertex’s stem-cell derived pancreatic islets for diabetes treatment.