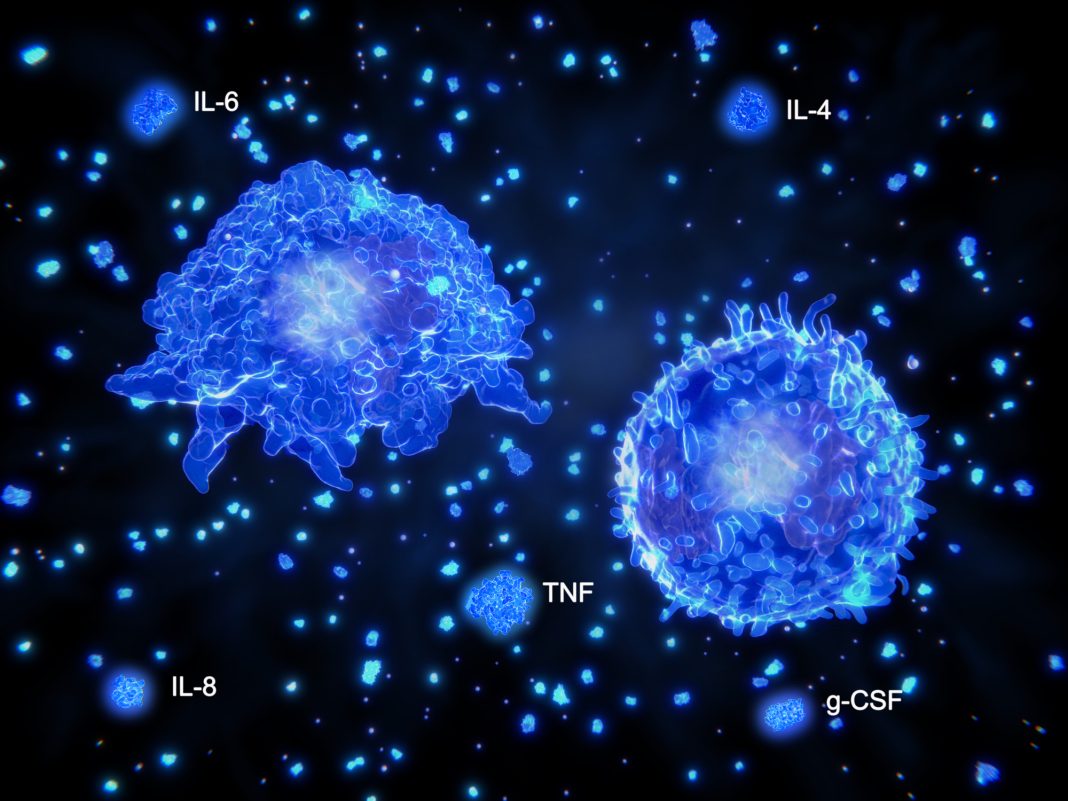
During some severe cases of COVID-19, a macrophage-induced cytokine storm occurs, which can lead to lasting tissue damage and poor patient outcomes. However, it is unclear how the SARS-CoV-2 infection induces the inflammatory response. Now, a new study outlines what controls the cytokine storm by lung-infiltrating macrophages, as these cells are not efficiently infected by SARS-CoV-2.
The study showed that the cytokine storm is linked to interferon (IFN-I) signaling in patient lungs. In addition, the findings point to the role of plasmacytoid dendritic cells (pDCs)—which are directly infected with SARS-CoV-2—as the main producers of IFN-I, which triggered TLR7 activation.
The authors presented a mechanism where pDCs are infected by SARS-CoV-2, subsequently produce IFN-I, and stimulate a macrophage-mediated cytokine storm during SARS-CoV-2 infection.
This work is published in Science Immunology in the paper, “Sensing of SARS-CoV-2 by pDCs and their subsequent production of IFN-I contribute to macrophage-induced cytokine storm during COVID-19.”
Type I interferons protect the host against SARS-CoV-2 infection, but may also have a deleterious effect. In addition, the source of IFN-I in the lungs of COVID-19 patients is not well understood.
The researchers found an infiltration of pDCs in the lungs of SARS-CoV-2–infected patients, which correlated with strong IFN-I signaling in lung macrophages. In addition, the researchers found that SARS-CoV-2 infects pDCs which results in a production of interferons that can provoke epigenetic changes in the nearby macrophages in the lungs of patients. This priming of macrophages by interferons leads to their exacerbated response to environmental stimuli, inducing the cytokine storm in the lungs of COVID-19 patients.
More specifically, the authors write that pDCs “were the main producers of IFN-I because they were directly infected with SARS-CoV-2, which triggered TLR7 activation. This IFN-I made macrophages more responsive to environmental stimuli, thus triggering the production of multiple cytokines.”
This is surprising as interferons and pDCs have been demonstrated to protect patients infected by SARS-CoV-2. But this new research uncovers that they can also provoke damaging cytokine storms.
In patients with severe COVID-19, they found that lung macrophages expressed a robust inflammatory signature, which correlated with persistent IFN-I signaling at the single-cell level. This led to the observation of an uncoupling of the infiltration of pDCs in the lungs and the associated IFN-I signature, with the cytokine storm in macrophages.
Further, they found that pDCs were the dominant IFN-α–producing cells in response to the virus in the blood, whereas macrophages produced IFN-α only when in physical contact with infected epithelial cells.
“There is still a lot we don’t know about the pathogenesis of COVID-19, and why macrophages can produce these cytokine storms that can have such dramatic consequences for patients,” said Franck Barrat, PhD, senior scientist at the Hospital for Special Surgery and professor of microbiology and immunology at Weill Cornell Medicine. “We hope that this research will bring us closer to that understanding and will lead to better treatment options for patients with severe COVID-19.”