It is common knowledge exercising is good for physical and mental health. Yet how physical activity affects the brain remains poorly understood in terms of mechanistic insights into the cellular and molecular pathways that connect physical activity to brain health.
A new study led by scientists at the University of California, San Francisco, (UCSF), Memory and Aging Center, on 167 decedents who were monitored for physical activity and cognitive function during life, and neuropathological markers at autopsy, provides insights on how physical activity may increase synaptic and cognitive resilience through a decrease in pro-inflammatory microglial states.

Kaitlin Casaletto, PhD, assistant professor at the UCSF Memory and Aging Center, and corresponding author of the study says, “Many studies show physical activity relates to better brain and cognitive health. For example, inactivity alone is estimated to account for 13% Alzheimer’s Disease cases worldwide. Yet, we still do not fundamentally understand the mechanisms linking physical activity to cognition in humans. Our study is the first human data showing that microglial activation (“brain inflammation”) may be a meaningful mechanism.”
The study is published in an article in the Journal of Neuroscience titled, “Microglial correlates of late life physical activity: Relationship with synaptic and cognitive aging in older adults.”
“Our team aims to identify biological targets that link known protective factors like physical activity to the brain. Ideally, if we can “bottle” these biological mechanisms, they could be therapeutic targets for cognitive aging and Alzheimer’s disease,” says Casaletto.
Microglia that account for nearly 15% of all cells found in the brain provide immune protection. They normally respond to neuronal damage by undergoing a reversible process of activation. Once activated, microglia can swallow damaged cells by a process called phagocytosis where their cell membranes extend to surround and destroy cellular debris, pathogens and other undesirable substances.
On the flip side, prolonged and intense microglial activation can trigger inflammation, damage neurons, and disrupt neural signaling. Chronic activation of microglia may release cytotoxic molecules such as proinflammatory cytokines, reactive oxygen intermediates, proteinases and complement proteins, causing neuronal death.
Animal and in vitro studies have shown exercise reduces aberrant activation of microglia, increases in the formation of connections between neurons (synaptogenesis) and the birth of new neurons (neurogenesis). But this link has not been established in humans until now.
In the current study, the researchers examined the relationship between physical activity and microglia activation in 167 older adults as part of the Rush Memory and Aging Project. Two-thirds of the participants did not suffer from dementia and 60% showed symptoms of Alzheimer’s disease (AD).
The participants wore activity monitors 24 hours a day for up to ten consecutive days before annual cognitive exams. In postmortem brain tissue analyses, the researchers measure morphological and synaptic markers of microglia activation and Alzheimer’s disease pathology through immunohistochemistry.
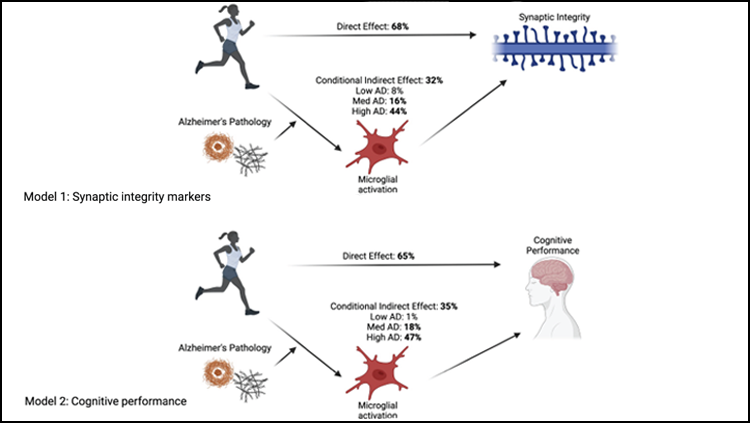
Based on their studies on this group, the researchers demonstrate greater physical activity is associated with a lower proportion of morphologically activated microglia (PAM) in the ventromedial caudate and the inferior temporal cortex, after adjusting for age, sex, education, and motor performances. The ventromedial caudate is associated with motor and procedural learning while the inferior temporal cortex, a region hit hardest in Alzheimer’s disease, is linked to visual processing and the neural representation of objects, places, faces, and colors.
“These are the first data supporting microglial activation as a physiological pathway by which physical activity relates to brain heath in humans. Though more interventional work is needed, we suggest that physical activity may be a modifiable behavior leveraged to reduce pro-inflammatory microglial states in humans,” the authors note.
Casaletto says, “We are starting to show the ‘who of the how’: physical activity related to better cognitive outcomes via reduced brain inflammation, particularly in adults with greater AD pathology. These findings support precision health approaches to preventative neurology. It is important to understand in whom and when interventions will be most efficacious. For example, physical activity may not work for everyone’s brain health.”
“A major limitation of this work is the observational design,” says Casaletto. “We cannot determine directionality of effects and it is likely that at least some of the relationship between physical activity and brain inflammation is bidirectional, i.e., brain inflammation leading to reductions in physical activity. We have an ongoing physical activity intervention study in which we hope to capture complementary markers of in vivo inflammatory markers to help support causality of effects.”
Also unknown are the forms, types and patterns of physical activity that reduce brain inflammation and improve cognition. Casaletto says, “We have ongoing analyses using Fitbit monitoring in older adults to capture minute-by-minute movement patterns to elucidate the patterns of physical activity that most strongly relate to brain health. We hope these lead to more precise recommendations.”
Future research from the group will also examine if physical activity interventions can alter microglia activation in AD patients. Working toward the goal of identifying biological pathways and novel molecules that link known protective lifestyle behaviors with cognitive health, “because these may be therapeutic (pharmacological) targets for cognitive aging/AD,” Casaletto and her team are collaborating with translational animal model investigators.
The study was supported by grants from NIH-NIA and the Alzheimer’s Association.



