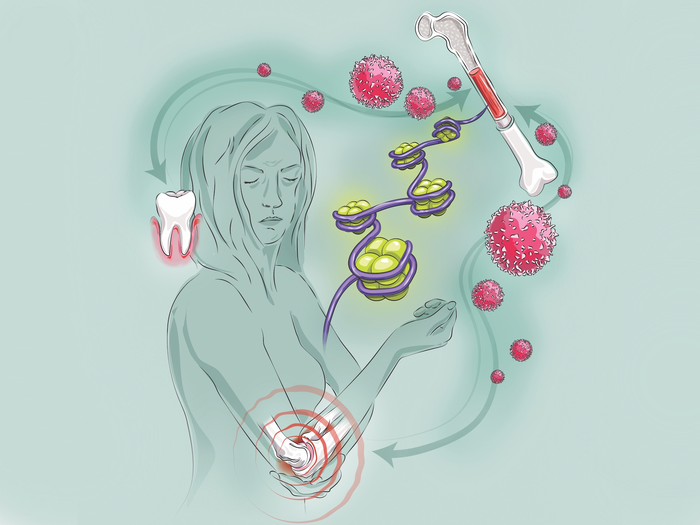
Innate immune memory can cause one type of inflammatory condition—for example, gum disease—to increase susceptibility to another—like arthritis. Now, new findings show that alterations to immune cell precursors in the bone marrow underlie the mechanism that forms the connection. Using a mouse model, the team demonstrated that recipients of a bone marrow transplant were predisposed to more severe arthritis if their donor had inflammatory gum disease.
This work is published in Cell in the article, “Maladaptive innate immune training of myelopoiesis links inflammatory comorbidities.”
“Although we use periodontitis and arthritis as our model, our findings go above and beyond these examples,” said George Hajishengalliis, DDS, PhD, professor at the University of Pennsylvania School of Dental Medicine. “This is in fact a central mechanism, a unifying principle underlying the association between a variety of comorbidities.”
In previous work, Hajishengallis and colleagues explored the role of innate immune memory. Their findings showed that the innate immune system’s myeloid cells, such as neutrophils and macrophages, could “remember” past encounters, becoming more responsive when exposed to a new threat. The work also showed that this “trained immunity” could be transferred from one organism to another through a bone marrow transplant, protecting recipients from cancer through an innate immune response.
The researchers hypothesized that this trained immunity could be detrimental in the right contexts. “The thoughts went like this: We knew the gum disease periodontitis increased the risk of comorbidities like cardiovascular disease,” said Hajishengallis. “And the reverse is also true: People with the inflammatory disease colitis, for example, have an increased prevalence of periodontal disease. Different mechanisms have been proposed, but no one unifying mechanism could explain this bidirectionality.”
The scientists sought the source of the association between comorbidities to the innate immune training they already knew was happening in the bone marrow.
The team showed that, within a week of inducing a mouse to have periodontal disease, the animal’s myeloid cells and their progenitor cells expanded in the bone marrow. Examining these cells weeks later, after periodontitis was intentionally resolved, the researchers did not notice significant changes in how the cells looked or behaved.
However, these progenitor cells appeared to have memorized the inflammation they were exposed to, as they harbored important epigenetic changes. The researchers found that these alterations, triggered by inflammation, could alter the manner in which the genes would be expressed after a future challenge. The overall pattern of epigenetic changes, the researchers noted, was associated with known signatures of the inflammatory response.
Mice with induced periodontal disease also had more severe responses to a later immune system challenge, evidence of trained immunity.
To put the whole picture together regarding the link between inflammatory conditions, the “critical experiment,” as Hajishengallis explained, was a bone marrow transplant. Mice that had periodontitis, a severe form of gum disease, served as donors, as did a group of healthy mice serving as controls. Two hundred stem cells from their bone marrow were transplanted into mice that had never had gum disease and which had had their own bone marrow irradiated. A few months later, these mice were exposed to collagen antibodies, which trigger arthritis.
“Mice that received the transplant from mice with periodontitis developed more severe arthritis than mice that received a donation of stem cells from periodontally healthy mice,” said Hajishengallis. In addition, higher joint inflammation in recipient mice was due to inflammatory cells deriving from the periodontitis-trained stem cells.
Further experiments suggested that the signaling pathway governed by a receptor for IL-1 played a vital role in contributing to this inflammatory memory. Mice that lacked IL-1 receptor signaling could not generate the immune memory that made the recipient mice more susceptible to comorbidities.
The work underscores that blocking IL-1 receptor signaling could be an effective approach to mitigate against these knock-on effects of trained immunity. “We’ve seen anti-IL-1 antibodies used in clinical trials for atherosclerosis with excellent results,” Hajishengallis said. “It could be that it was in part because it was blocking this maladaptive trained immunity.”
Follow-up projects are examining how other inflammatory conditions, may be linked with periodontal disease, a sign, the researchers said, of how crucial oral health is to overall health.