Natural killer cells don’t have to be natural born natural killer cells. In fact, mass produced natural killer cells—that is, natural killer (NK) cells derived from induced pluripotent stem cells (iPSCs)—can be more persistent, more effective killers, reported scientists based at the University of California, San Diego (UCSD). These scientists say that one way to turn human iPSC-derived NK cells into uninhibited killing machines is to deprive them of a gene that encodes a crucial cytokine regulator.
Details about human iPSC-derived NK cells appeared in an article in Cell Stem Cell. The cells lack a gene called CISH, which encodes cytokine-inducible SH2-containing protein, a checkpoint or braking mechanism that is ordinarily expressed by NK cells that are stimulated by cytokines such as interleukin-15 (IL-15). Without this braking mechanism, NK cells can go on a killing spree.
According to experimental evidence, the human iPSC-derived NK cells have greater cytotoxic activity in vitro. They are also better at inhibiting tumor progression in vivo. Finally, they display greater metabolic fitness—just the thing to keep a killing spree going.
The article, titled “Metabolic Reprogramming via Deletion of CISH in Human iPSC-Derived NK Cells Promotes In Vivo Persistence and Enhances Anti-tumor Activity,” was contributed by a team of scientists led by Dan Kaufman, MD, PhD, professor of medicine in the division of regenerative medicine and director of cell therapy at UCSD School of Medicine.
“We found that CISH-deleted iPSC-derived NK cells were able to effectively cure mice that harbor human leukemia cells, whereas mice treated with the unmodified NK cells died from the leukemia,” said Kaufman, who is also a faculty member of both the Sanford Consortium for Regenerative Medicine and the Sanford Stem Cell Clinical Center at UCSD Health. “These studies demonstrate that we can now edit iPSC-derived NK cells to remove an inhibitory gene inside the cell to improve activation of NK cells.
“We demonstrate that the CISH deletion improves NK cell function in at least two different ways. First, it removes a brake on IL-15 signaling, which improves NK cell activation and function, even at low IL-15 concentrations. Second, it leads to metabolic reprogramming of the NK cells. They become more efficient at energy utilization, which improves their function in vivo.”
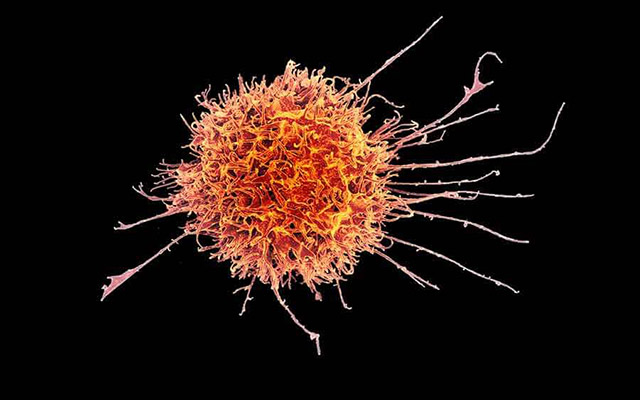
NK cells are lymphocytes in the same family as T and B cells, and are part of the innate immune system. They circulate throughout the body and are among the first to respond to the presence of foreign cells or invaders, most notably viruses and early signs of cancer. As such, they hold great promise as the basis for anticancer therapies, able to identify and target malignant cells, but their efficacy has proven limited.
To advance the potential held by NK cells, Kaufman and colleagues reprogrammed skin or blood cells to become iPSCs, which were then directed to become NK cells. This strategy produces a standardized cell population, rather than needing to isolate cells on a patient-specific basis.
Next, the researchers deleted the CISH gene in the iPSC-derived NK cells. Lacking this gene, the iPSC-derived NK cells demonstrated increased IL-15-mediated JAK-STAT signaling, a mechanism that alerts immune system cells, such as macrophages, lymphocytes, and fibroblasts to sites of infection, inflammation, and trauma.
“Consequently, CISH−/− iPSC-NK cells exhibit improved expansion and increased cytotoxic activity against multiple tumor cell lines when maintained at low cytokine concentrations,” the authors of the Cell Stem Cell article wrote. “CISH−/− iPSC-NK cells display significantly increased in vivo persistence and inhibition of tumor progression in a leukemia xenograft model.
“Mechanistically, CISH−/− iPSC-NK cells display improved metabolic fitness characterized by increased basal glycolysis, glycolytic capacity, maximal mitochondrial respiration, ATP-linked respiration, and spare respiration capacity mediated by mammalian target of rapamycin (mTOR) signaling that directly contributes to enhanced NK cell function.”
Kaufman and colleagues are now working to translate the findings into a clinical therapy. “As iPSC-derived NK cells are now in clinical trials to treat both hematologic (blood) malignancies and solid tumors, we expect that CISH-deleted iPSC-NK cells can provide an even more effective treatment,” Kaufman stated. “Importantly, iPSCs provide a stable platform for gene modification, and since NK cells can be used as allogeneic cells that do not need to be matched to individual patients, we can create a line of appropriately modified iPSC-derived NK cells suitable for treating hundreds or thousands of patients as a standardized, off-the-shelf therapy.”