Immunotherapy can be very successful against some types of cancer, but its effectiveness against pancreatic tumors is limited, and also differs between men and women. Researchers at Karolinska Institute have now found a possible explanation for this sex difference. Their studies identified in women with pancreatic cancer, the presence of a population of immune cells that highly expresses a protein called FPR2, and which obstructs the body’s immune response. Tests in mouse models showed that knocking out FPR2 on these macrophages held back tumor growth in female mice. The results, the researchers suggest, indicate that FPR2 has an immunosuppressive function in pancreatic cancer, could feasibly offer up a new, sex-specific immunotherapy strategy against the disease.
“More and more evidence is coming in that male and female hormones affect our immune system, but much remains to be done before sex can be included as a self-evident biological factor in medical research and therapy,” said Fei He, PhD, a former visiting researcher at the Department of Laboratory Medicine, Karolinska Institutet, who is first author of the team’s published paper in Cancer Research. “Our results provide new perspectives that can have high impact on the treatment of cancer.
He, together with research lead Dhifaf Sarhan, PhD, an assistant professor at the Karolinska Institutet Department of Laboratory Medicine, and colleagues, reported on their studies in a paper titled “FPR2 shapes an immune-excluded pancreatic tumor microenvironent and drives T-cell exhaustion in a sex-dependent manner,” in which they concluded, “Overall, this study identified an immunosuppressive function of FPR2 in females, highlighting a potential sex‐specific precision immunotherapy strategy.”
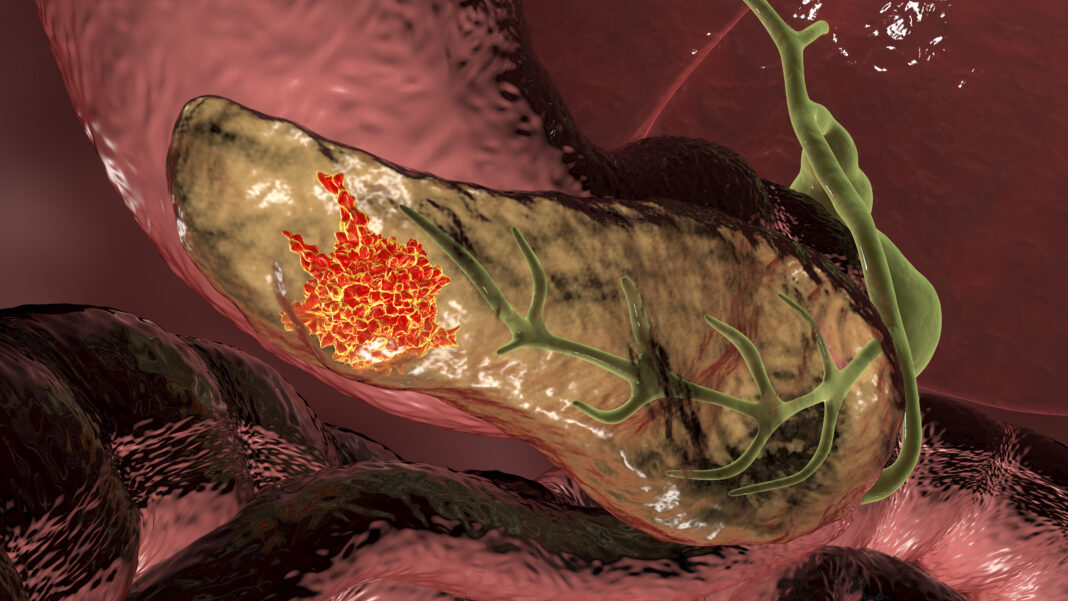
Pancreatic ductal adenocarcinoma (PDAC) is almost universally fatal, the authors wrote, and patients live on average four to six months after diagnosis. About 20% of pancreatic cancer patients may be suitable for surgery and chemotherapy, which can raise five-year survival to 30–58%, but PDAC still remains “amongst the most deadly form of cancer types.” Diagnosis is commonly made when patients already have advance disease and treatment options are limited.
Immunotherapy is designed to stimulate the immune system to attack cancer cells, and in recent years has contributed significantly to the treatment of different kinds of cancer, such as melanoma and lung, kidney and liver cancer. “Immunotherapy has developed rapidly in the last two decades and has gradually become an effective treatment method that can be operated in the clinic by regulating the switch of the immune system to fight tumors,” the authors wrote. However, immunotherapy is far less effective against pancreatic cancer. “This observed immunotherapy disappointment” in pancreatic cancer has been linked to the cancer’s complex immunosuppressive environment, the investigators continued. “The dysfunction of cytotoxic immune cells is linked to the accumulation of tumor-associated macrophages (TAMs), contributing to a dense stroma, accompanied by immune cell exhaustion and limited effector cell infiltration.”
Previous studies have shown that there are sex-related biological differences in the male and female immune system that, amongst other effects, determine how tumors grow and the body’s ability to defend itself against them. “Sex-driven immune differences can affect tumor progression and the landscape of the tumor microenvironment,” the investigators noted. However, they acknowledged, “There remains a huge knowledge gap about the differential response to immunotherapy between sexes.”
For their study, the researchers carried out a number of analyses and experiments, including single-cell RNA sequencing, proteomics, test tube and patient validation, and experiments that aimed to test potential therapeutic strategies, using 3D pancreatic cancer models and live mice. The results highlighted a key difference in tumor properties between and women with pancreatic cancer, as well as pointing to therapeutic strategies. The collective study results demonstrated the presence, in females, of a strongly immunosuppressive subpopulation of tumor-associated macrophages that express FPR2, and which promoted inhibition of T cells and natural killer cells. These cells, the results suggest, effectively protect the tumor, prevented the immune system’s T cells from infiltrating the tumor and attacking the cancer cells.
Initial analyses using human-derived samples indicated that FPR2 expression on these myeloid cells is associated with a suppressive myeloid profile and worse tumor progression, but specifically in female PDAC patients. “This sub-group of immune cells correlates with poor survival exclusively in female cancer patients,” said Sarhan.
Further experiments showed that the growth of pancreatic tumors was suppressed significantly in FPR2 knockout (KO) female mice when compared with knockout male mice, or normal, wild-type animals. Inoculating tumors with FPR2 KO macrophages also significantly reduced tumor growth, again, in female mice.
The combined study results could help direct the development of diagnostic tools and immunotherapy strategies for pancreatic cancer that take into account biological differences between men and women, the team suggests. “FPR2 is a sex-dependent mediator of macrophage function in pancreatic cancer and can be targeted to reprogram macrophages and stimulate anti-tumor immunity in females,” the authors wrote.
Sarhan added, “Our results show that the immune cells express a specific protein called FPR2 and can serve both as a sex-specific prognostic factor and a therapeutic target. The next step is to follow up our new immunotherapy target for women. We’re also performing extensive analyses to understand how immunological sex differences drive tumor development in different ways in male and female cancer patients with the goal to find and develop immunotherapy targets for each group.”
As the researchers concluded in their paper, “Our study indicates that reprogramming of TAMs represents a strategy to rescue T cell exhaustion in the tumor immune microenvironment and to convert the immunosuppressive milieu.” These mechanisms may include consideration of immunotherapy strategies for pancreatic cancer by stratifying according to patient sex.
“Additionally, our results suggest that modulation of the immune environment by synthetic drugs may reprogram women’s immunosuppressive TME and confer potential immune checkpoint therapeutic opportunities,” they pointed out. “Deeper understanding of the selective pressures and mechanisms of immune escape in tumors in males and females can inform patient selection strategies and can be utilized to further improve immunotherapy approaches in cancer.”