When a tissue experiences inflammation, its cells develop a memory that then equips them to react quickly and broadly in the event of second, future threat, even if the nature of that subsequent assault is different. The phenomenon, which is known as inflammatory memory, or “trained immunity,” has been recognized for nigh on 100 years, but the underlying mechanisms have remained elusive.
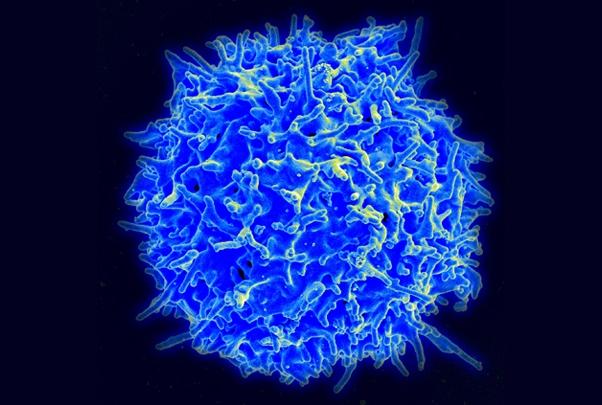
Using mouse epidermal stem cells as a model, scientists at the Rockefeller University have now unraveled the mechanism behind trained immunity, and elucidated how cells establish, maintain, and recall inflammatory memory. Their results suggest that this mechanism may be universal across diverse cell types, but may also not always be welcome. “This is happening in natural killer cells, T cells, dendritic cells from human skin, and epidermal stem cells in mice,” said Samantha B. Larsen, PhD, a former graduate student in the laboratory of Elaine Fuchs, PhD, the Rebecca C. Lancefield professor at the Rockefeller University. “The similarities in mechanism are striking, and may explain the remitting and relapsing nature of chronic inflammatory disorders in humans.”
Reporting on their findings in Cell Stem Cell (“Establishment, maintenance, and recall of inflammatory memory”), the team concluded, “While additional studies will be needed to challenge the universality of this model, our findings provide a compelling explanation for a phenomenon that has remained much of a mystery for the past 100 years.”
Trained immunity endows cells with the ability to respond more rapidly and robustly to a wide variety of secondary assaults, the authors explained. Pinning proteins to its genetic material at the height of inflammation, the cells effectively bookmark where they left off, so when they are subjected to attack at some future time-point, this inflammatory memory kicks in. The cells draw from their prior experience to respond more efficiently, even to threats that they have not encountered before. For example, skin heals a wound faster if it was previously exposed to an irritant, such as a toxin or pathogen; immune cells can attack new viruses after a vaccine has taught them to recognize just one virus. “It has long been known that plants and invertebrates acquire broad resistance to a range of pathogens if they survive one serious bout,” the scientists wrote. “Similarly, in the early 1930s, physicians noticed that mortality rates arising from virulent Mycobacterium tuberculosis and other dangerous pathogens plummeted when neonates were vaccinated for bacillus Calmette-Guérin (BCG).”
When thinking about our immune system we tend to default to considering the specific immunity that is mediated by the body’s T cells and B cells, which are trained by experience or vaccination to remember the specific contours of the last pathogen that they encountered. In contrast, while trained immunity represents a less specific strategy, it is available to many cells, and allows the cells to respond to entirely new threats by drawing on general memories of inflammation. The impact is shorter-lived, but broader in scope.
Scientists have long suspected that even cells that are not traditionally involved in the immune response have the rudimentary ability to remember prior insults and learn from experience. In 2017, the Fuchs lab published research demonstrating that mouse skin that had recovered from irritation healed 2.5 times faster than normal skin when exposed to irritation at a later date.
One explanation, the Fuchs team proposed, could be epigenetic changes to the skin cell genome itself. During inflammation, regions of DNA that are usually tightly coiled around histone proteins unravel to transcribe a genetic response to the attack. Even after the dust settles, a handful of these memory domains remain open, and changed. Some of their associated histones have been modified since the assault, and transcription factor proteins have latched onto the exposed DNA. A once-naïve cell is effectively prepared for the next assault.
Despite what was already understood, the molecular mechanism that explained this process, and how the cell could use it to respond to types of inflammation and injury that it had never previously encountered, remained a mystery.
For their newly reported research the Fuchs lab once again exposed mice skin to irritants, and watched as stem cells in the skin changed. “We focused on the regions in the genome that become accessible during inflammation, and remain accessible afterwards,” said Christopher Cowley, a graduate student in the Fuchs lab. “We call these regions memory domains, and our goal was to explore the factors that open them up, keep them open, and reactivate them a second time.” The authors further explained, “Memory domains are classically defined as chromatin regions that gain accessibility during the inflammatory response and remain so following resolution.”

Further experiments unveiled a two-step mechanism at the heart of trained immunity. The process revolves around transcription factors (TFs)—proteins that govern the expression of genes—and hinges on the twin transcription factors known as JUN and FOS.
The mechanism involves an initial response by the stimulus-specific STAT3 transcription factor, which is deployed to coordinate a genetic response to a particular genre of inflammation. This protein then hands the baton to JUN-FOS, which perches on the unspooled genetic material. The specific transcription factor that sounded the original alarm will eventually disappear, and FOS will float away as the tumult quiets down. But JUN remains to effectively guard the open memory domain with another set of transcription factors, waiting for the next insult.
Then, when irritation strikes again, JUN is ready. It rapidly recruits FOS back to the memory domain, and the duo trigger the response. This time, no specific transcription factor is necessary to respond to a particular type of inflammation, rather, the system unilaterally activates in response to virtually any stress.
The researchers say that by demonstrating that rapid reactivation of memory-associated genes is dependent upon FOS, the data suggest that JUN may act as “a sentinel,” that makes memory recall and gene reactivation possible in response to a range of secondary stimuli.
“We unearth an essential, unifying role for the general stress-responsive transcription factor FOS, which partners with JUN and cooperates with stimulus-specific STAT3 to establish memory; JUN then remains with other homeostatic factors on memory domains, facilitating rapid FOS re-recruitment and gene re-activation upon diverse secondary challenges,” they explained. “By invoking an obligatory two-step mechanism for memory establishment, one involving a context-specific TF that can specify the opening of chromatin in memory domains and the other involving FOS-JUN for chromatin remodeling and transcription, the stage is set for binding of stem cell factors and maintaining an open chromatin state in the absence of transcription.”
Trained immunity may sound like a boon to human health, with veteran immune cells seeming to produce broader immune responses. But the generalized reaction may not always benefit the rest of the body. The same mechanism that keeps cells on high alert may instill a sort of molecular paranoia, in chronic inflammation disorders. “Irrespective of cell type, inflammatory memory enables an altered response to a broadened range of stressors and can be adaptive or maladaptive, leading to improved tissue fitness or chronic inflammatory disorders, respectively,” the investigators commented.
When the Fuchs lab examined data collected from patients who suffer from systemic sclerosis, for instance, they found evidence that JUN may be sitting right on the memory domains of affected cells, poised to incite an argument in response to even the slightest disagreement.
The scientists hope that shedding light on one possible cause of chronic inflammatory disease may help researchers develop treatments for these conditions. “The factors and pathways that we identify here could be targeted, both in the initial disease stages and, later, during the relapsing stages of disease,” said Cowley. Larsen added: “Perhaps these transcription factors could be used as a general target to inhibit the recall of the memories that cause chronic inflammation.”


