Hemophilia B is a rare X-chromosome-linked bleeding disorder caused by mutations in the blood clotting factor IX that reduce its circulating levels in blood. A clinical trial led by experts at the University College London (UCL), the Royal Free Hospital, and Freeline Therapeutics, a clinical-stage biotechnology company, has tested the safety and efficacy of a liver-directed gene therapy to restore factor IX levels long-term in hemophilia B patients.
The team published their results of the phase I/II trials on July 20, 2022, in the New England Journal of Medicine “Phase 1–2 Trial of Gene Therapy for Hemophilia B“.
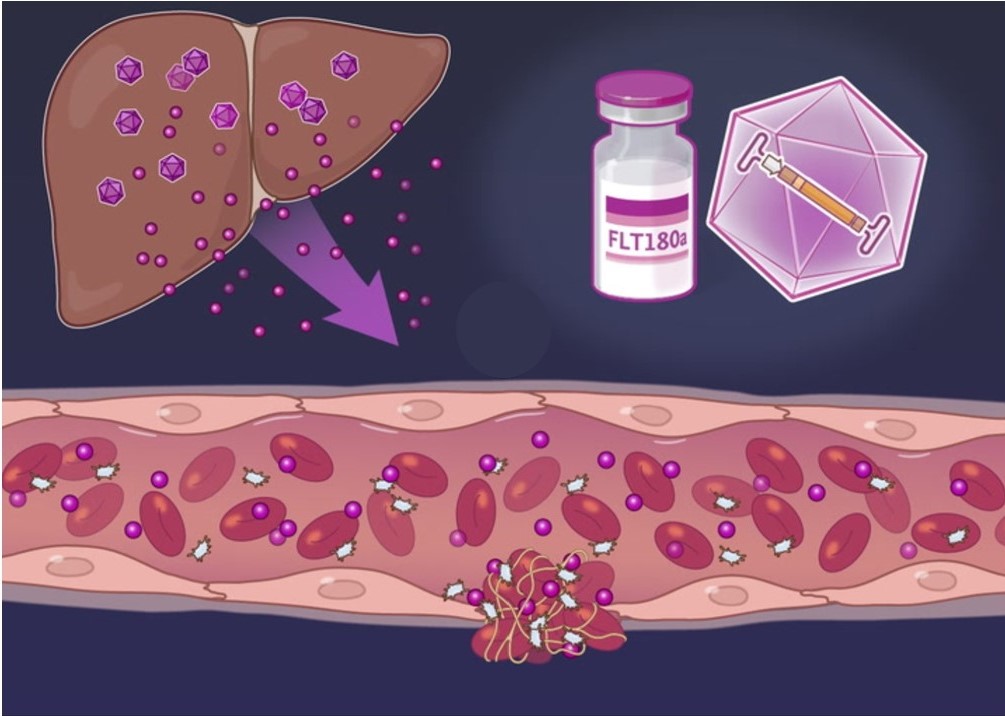
The team continues to evaluate the adeno-associated virus (AAV) based gene therapy candidate, called FLT180a, for the treatment of patients with severe and moderately severe hemophilia B, with less than 2% factor IX compared to normal values. If successful, a single injection of FLT180a could radically reduce bleeding risks in individuals living with hemophilia B. The gene therapy uses a synthetic viral capsid and a gain-of-function protein to boost factor IX levels long-term.
At present, treatment for patients with hemophilia B—who are mostly men, since it is an X-linked genetic disease—involves weekly injections of recombinant clotting factor IX. This regular ‘replacement therapy’ maintains threshold levels factor IX to prevent excessive bleeding. However, this approach does not prevent debilitating arthritis and joint damage due to chronic inflammation of the synovial lining when blood accumulates in a joint and corrodes the articular cartilage.
The multi-center, open-label, phase I/II clinical trial called B-AMAZE, and the related long-term follow up study, found that a one-time injection with FLT180a sustained synthesis of normal levels of factor IX protein in the liver in nine of ten patients, across four doses, precluding the need for regular replacement therapy.
As part of the 26-week trial, ten patients received one of four FLT180a doses that ranged from 3.84×1011 to 1.28×1012 vector genomes per kilogram of the patient’s body weight. After 26 weeks, five patients had normal levels of factor IX protein, three had low but increased levels, and one patient who received the highest dose had an abnormally high level. Upon reaching the primary end points of safety and efficacy at week 26, all ten patients were included in a 15-year long-term follow up that will assess the safety and durability of factor IX expression.
Pratima Chowdary, MD, professor at Royal Free Hospital, UCL Cancer Institute and lead author of the study said, “Removing the need for hemophilia patients to regularly inject themselves with the missing protein is an important step in improving their quality of life. The long-term follow-up study will monitor the patients for durability of expression and surveillance for late effects.”
All patients in the trial were also required to take immune suppressing drugs (glucocorticoids with or without tacrolimus) over several weeks to months, to prevent their immune systems from mounting an attack against the viral vector which could lead to rejection of the therapy.
Overall, the treatment was well tolerated. However, all patients experienced some adverse events. An abnormal blood clot was detected in one patient who received the highest FLT180a dose and had the highest levels of factor IX protein.
“Gene therapy is still a young field that pushes the boundaries of science for people with severe genetic diseases,” Amit Nathwani, PhD, professor at UCL Medical Sciences and co-founder of Freeline said. “The B-AMAZE long-term data add to the growing body of evidence that gene therapy has the potential to free patients from the challenges of having to adhere to lifelong therapy or could provide treatment where none exists today.”
Pamela Foulds, MD, Chief Medical Officer of Freeline, said, “The B-AMAZE long-term data continue to support our confidence that a single dose of FLT180a could protect people with hemophilia B from bleeding and the need for lifelong factor IX replacement through durable expression of factor IX at protective levels.”
Geraint Rees, PhD, professor and Vice-Provost Research, Innovation and Global Engagement, and Non-Executive Director at UCL Business said, “The results of this important study are a perfect example of how UCL research and innovation can translate to real-world and life-changing impact.”
Based on the phase I/II trial, the authors concluded low doses of FLT180a sustained factor IX levels in the normal range but necessitated immunosuppression.