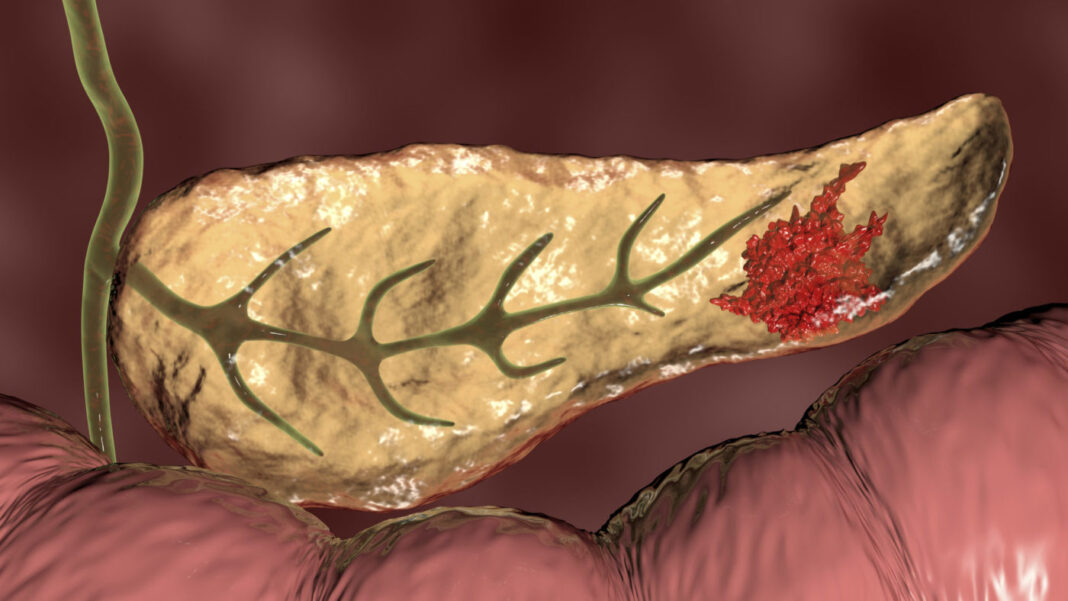
Researchers at the University of Toronto (U of T) and University Health Network (UHN) have shown how probiotic Lactobacillus bacteria in the gut could undermine immunity in pancreatic cancer and spur cancer growth, by impacting on the function of macrophages in the pancreatic tumor microenvironment (TME). The results, they suggest, could point toward more personalized cancer treatments.
The newly reported studies showed that Lactobacillus—a type of bacteria thought to promote gut health—affects macrophage function through the metabolization of dietary tryptophan (Trp), an essential amino acid found in protein from plant- and animal-based foods. The team’s experiments demonstrated that the metabolites resulting from microbial tryptophan metabolization activate the aryl hydrocarbon receptor (AHR) in macrophages, tissue-resident immune cells thought to play an important role in tumor growth and metastasis. Their results also indicated that levels of AHR correlated with progression of pancreatic ductal adenocarcinoma (PDAC), immune suppression, and patient survival.
“Most studies focus on positive correlations between the microbiome and cancer outcomes,” said Tracy McGaha, PhD, a professor of immunology at U of T’s Temerty Faculty of Medicine and a senior scientist at Princess Margaret Cancer Centre, UHN. “This work focused on negative correlations of the microbiome with cancer, and suggests that in some conditions, the constituency of the microbiome may have a negative impact.” McGaha and colleagues reported on their findings in Immunity, in a paper titled, “Tryptophan-derived microbial metabolites activate the aryl hydrocarbon receptor in tumor-associated macrophages to suppress anti-tumor immunity,” in which they concluded, “Ultimately, the data suggest that dietary Trp is a key driver of immune phenotype in the PDAC TME by serving as a source of indoles via microbiome metabolization … Thus, microbial metabolites activate AHR in macrophages, driving macrophage polarization and PDAC outcomes.”
Pancreatic cancer is the third-most deadly cancer in Canada, despite being relatively rare, the authors noted. Patients with the disease have not seen the same improvements in survival that have been witnessed in other cancers over the last three decades. As such, and despite key improvements in cancer therapies, outcomes for patients with pancreatic ductal adenocarcinoma remain “grim,” as this form of cancer demonstrates resistance to treatment approaches including checkpoint blockade.
Patient microbiota appear to impact PDAC outcomes, the team added. “In long-term PDAC survivors, increased microbiome diversity correlates with survivorship and immunologic features of the TME.” Reported fecal transplantation studies in mouse models have also indicated that the microbiota can promote or inhibit tumor progression and impact TME cellular composition.
Indoles, a class of metabolites resulting from microbial tryptophan metabolization, activate the AHR, a protein that regulates gene expression, and which can enable both beneficial inflammation and immune suppression in other areas of the body. “The AHR is a sensor of products of tryptophan metabolism and a potent modulator of immunity,” the investigators noted.
Their newly reported studies showed that deletion or inhibition of AHR in tumor-associated macrophages (TAM) led to reduced growth of pancreatic cancer, better sensitivity to treatments, and increased numbers of inflammatory T cells. “…we deleted AHR in PDAC TAMs or inhibited AHR activity pharmacologically,” they wrote. “Loss of AHR function caused a reduction in tumor size, and AHR-deficient TAMs acquired a proinflammatory phenotype with increased intra-tumoral IFNγ+CD8+ T cells.” Conversely, activation of AHR thwarted these beneficial effects.

Interestingly, microbial production of indole compounds was found to be the key driver of AHR activity. McGaha said he was surprised the microbiome had such a strong impact on AHR and immune function. “We weren’t thinking about the microbiome at first, we were just interested in AHR as a factor in the tumor microenvironment,” McGaha said. “But when we blocked the mammalian genes that can activate AHR, it had no effect.”
The researchers were then prompted to look at Lactobacillus, partly because previous studies had shown that the bacteria correlated with AHR activity and reduced inflammation, both of which can enable cancer growth. For their newly reported work the team, in collaboration with Dana Philpott, PhD, also a professor of immunology, tested the effects of the bacteria in mice with surgical models of pancreatic cancer.
They also moved the project forward with single-cell analysis—a technology that provides genome-scale data on individual cells. “… it’s been invaluable for us to see population responses in the gene expression patterns of macrophages and other immune cells, and what’s going on around them,” McGaha added.
The researchers in addition carried out tests with human tissue samples and analyzed data from human trials. Their findings indicated that high expression of AHR correlated with disease progression, immune suppression, and patient survival. “In human PDAC samples, AHR expression was associated with rapid disease progression and mortality, as well as with an immune-suppressive TAM phenotype,” the team noted. “Pan-cancer analysis showed that PDAC exhibits higher AHR compared with most other cancer types … In PDAC patients, AHR expression below the median value was associated with improved overall survival (OS) compared with patients above the median.”
To help address the urgent need for more effective treatments, McGaha is working with clinician scientists at UHN on a clinical trial called PASS-01. The study is a collaboration with other Canadian and U.S. cancer centers that aims to uncover personalized predictors of patient response to chemotherapy. The team will collect stool samples before and after chemotherapy to look for enrichment of Lactobacillus, and whether the bacteria correlates to treatment response, patient survival, and their observations on how it acts in the tumor environment. “It’s exciting as a basic scientist to be involved in translational research, and it’s been nice to see the physician scientists interested in this work,” McGaha said.
As the authors further pointed out, “… a first-in-human clinical trial targeting AHR has been initiated in patients with advanced solid lung, colorectal, and urothelial tumors (clinicalTrials.gov identifier: NTC04069026), indicating potential applicability of AHR inhibition in multiple cancer types. Ultimately, these trials will provide a definitive test as to whether AHR is a legitimate target for cancer therapy.”
Longer term, the McGaha lab will look to gain a deeper understanding of how immune cells interact with the microbiome. “The link we identified between AHR, immune function, indoles, and microbiome constituents may provide useful prognostics for predicting patient outcomes,” they further suggested. “Our results suggest that targeting immunologic responses to the microbiome could have meaningful impact on therapy, augmenting microbiome manipulation approaches or potentially bypassing the need to manipulate the microbiome by precise inhibition of the response to microbial metabolites.”
The hope is to improve on promising therapies such as fecal microbiota transplants—which have been hampered by the complexity and variety of gut bacteria—or to try a new approach. “It could be possible to bypass the need to manipulate the microbiome, through precise targeting of the immune response to microbial metabolites,” said McGaha. “That’s a cool new direction we’d like to explore.”