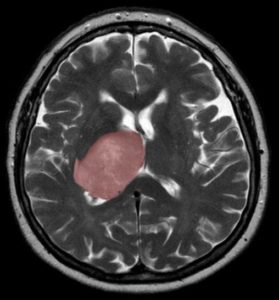
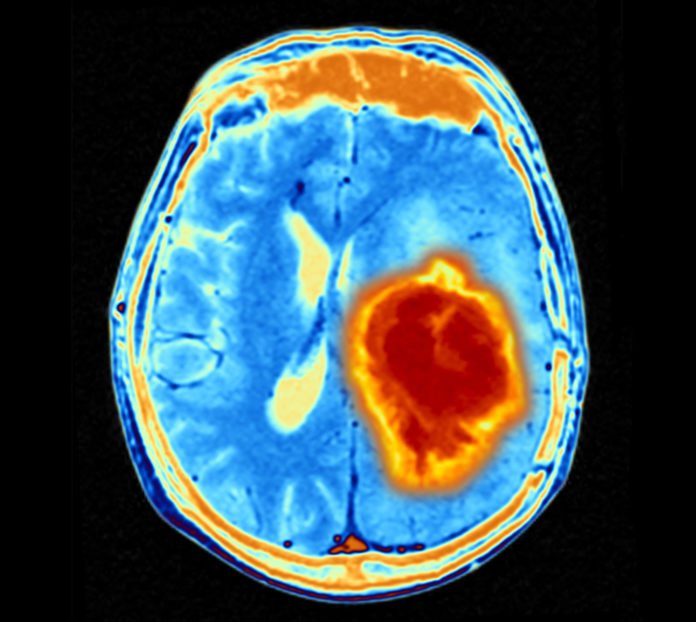
The results of studies by researchers in Canada suggest that the healing process that follows a brain injury—such as trauma, infection or stroke—could spur the growth of glioblastoma tumors, when new cells generated to replace those lost to the injury are derailed by mutations. The findings, reported by an interdisciplinary team of researchers at the University of Toronto, The Hospital for Sick Children (SickKids) and the Princess Margaret Cancer Centre, could lead to the development of new approaches to treating glioblastoma, which is one of the most difficult-to-treat brain cancers in adults.
“Our data suggest that the right mutational change in particular cells in the brain could be modified by injury to give rise to a tumour,” said Peter Dirks, MD, PhD, who is Head of the Division of Neurosurgery and a Senior Scientist in the Developmental and Stem Cell Biology program at SickKids. “Glioblastoma can be thought of as a wound that never stops healing. We’re excited about what this tells us about how cancer originates and grows and it opens up entirely new ideas about treatment by focusing on the injury and inflammation response.”
The researchers, headed by Dirks, and by Gary Bader, PhD, a professor of molecular genetics in the Donnelly Centre for Cellular and Biomolecular Research at U of T’s Temerty Faculty of Medicine, and Trevor Pugh, PhD, senior scientist at the Princess Margaret, reported their findings in Nature Cancer, in a paper titled, “Gradient of Developmental and Injury Response transcriptional states defines functional vulnerabilities underpinning glioblastoma heterogeneity.” Dirks is a Dream Team leader for the pan-Canadian Stand Up To Cancer Canada Dream Team that is focused on glioblastoma.
Glioblastoma is one of the most aggressive and treatment-refractory brain tumors in adults, the authors stated. Glioblastoma patients currently have limited treatment options available to them, and an average lifespan of just 15 months after diagnosis. “Treatment failure is rooted in the extensive heterogeneity observed within tumors and across patients,” the team further commented. “Glioblastomas harbor diverse cell populations, including rare glioblastoma stem cells (GSCs) that drive tumorigenesis.”
Dirks’ team had previously shown that GSCs are responsible for tumor initiation and recurrence after treatment, and for their reported studies, the team aimed to characterize the diversity within this GSC fraction. To do this they applied the latest single-cell RNA sequencing and machine learning technologies to map the molecular make-up of GSCs cultured from the tumors of 26 patients.
The team expanded the patient-derived GSCs in the lab to obtain sufficient numbers of the rare cells for analysis. Almost 70,000 cells were analyzed using the single-cell RNA sequencing technology, which detects what genes are switched on in individual cells. This effort was led by co-author Laura Richards, a graduate student in Pugh’s lab.
The resulting data confirmed extensive disease heterogeneity, meaning that each tumor contains multiple subpopulations of molecularly distinct cancer stem cells, making recurrence likely, as existing therapy can’t wipe out all the different subclones. “The goal is to identify a drug that will kill the glioblastoma stem cells,” noted Bader, whose graduate student Owen Whitley, contributed to the computational data analysis. “But we first needed to understand the molecular nature of these cells in order to be able to target them more effectively.”
A closer look revealed that each tumor exhibited either of two distinct molecular states—which the authors termed “Developmental” and “Injury Response”—or was somewhere on a gradient between the two. The Developmental state represents a hallmark of the glioblastoma stem cells and resembles that of the rapidly dividing stem cells in the growing brain before birth. The second state came as a something of a surprise to the researchers, who gave it the description Injury Response because it showed an upregulation of immune pathways and inflammation markers, such as interferon and TNFalpha, which are indicative of wound healing processes. These immune signatures were picked up by the single-cell technology, but were missed by older methods for bulk cell measurements.
Additional experiments led by Stephane Angers’ lab at the Leslie Dan Faculty of Pharmacy established that the two states are vulnerable to different types of gene knock outs, revealing a swathe of therapeutic targets linked to inflammation that had not been previously considered for glioblastoma.
The studies also found that the relative comingling of the two states was patient specific, such that each tumor was biased either toward the Developmental or toward the Injury Response end of the gradient. “While GSCs from each patient were composed of multiple transcriptionally and genetically distinct subpopulations, all GSCs converged on a single biological axis, spanning two recurrent cell states defined by neurodevelopmental and inflammatory programs,” the investigators noted.
They are now looking to target these biases for tailored therapies. “… the heterogeneity we have discovered at the GSC level suggests that therapies must be developed to simultaneously target both developmental and inflammatory processes observed in GBMs and GSCs.” Pugh, who is also the Director of Genomics at the Ontario Institute for Cancer Research, explained, “We’re now looking for drugs that are effective on different points of this gradient. There’s a real opportunity here for precision medicine—to dissect patients’ tumors at the single cell level and design a drug cocktail that can take out more than one cancer stem cell subclone at the same time.”
As the authors concluded, “We propose that glioblastomas grow out of a fundamental GSC-based neural wound response transcriptional program, which is a promising target for new therapy development … Our work provides a model that explains the source of cellular heterogeneity in GBMs and identifies a range of sensitivities of this fundamental cellular program that directly inform the development of new therapeutic strategies targeting GBMs.”


Comments are closed.