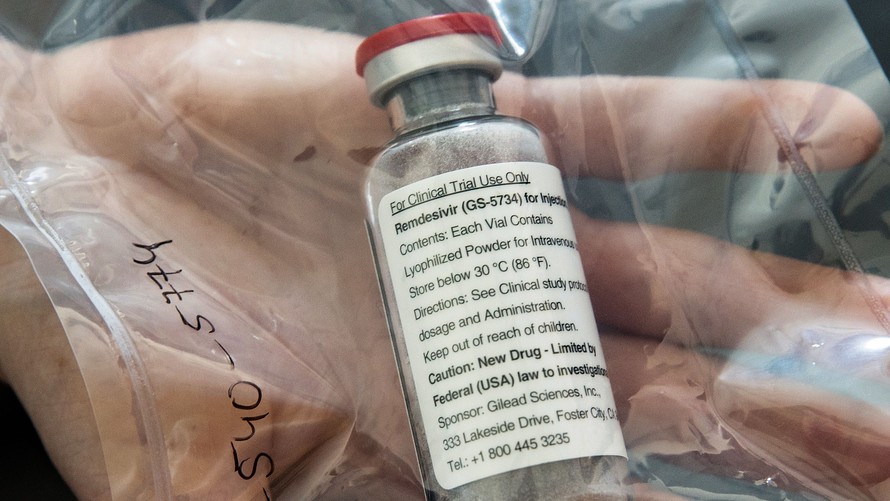
Eight months after it was first tested in human patients at the center of the world’s first COVID-19 outbreak, Gilead Sciences’ antiviral remdesivir yesterday won the FDA’s first approval of a drug against the virus—but for a smaller population than allowed under its previous emergency use authorization (EUA) from the agency.
Remdesivir—to be marketed in the United States as Veklury®—will be indicated for adults and pediatric patients 12 years of age and older who have forms of COVID-19 serious enough to require hospitalization, and who weigh at least 40 kg (88 pounds).
“Since the beginning of the COVID-19 pandemic, Gilead has worked relentlessly to help find solutions to this global health crisis. It is incredible to be in the position today, less than one year since the earliest case reported of the disease now known as COVID-19, of having an FDA-approved treatment in the United States that is available for all appropriate patients in need,” Gilead chairman and CEO Daniel O’Day said in a statement.
The FDA approval does not extend to children under age 12 who are hospitalized with COVID-19 and who weigh between 3.5 kg (7.7 pounds) and 40 kg (88 pounds) because clinical trials in that subpopulation of patients remain ongoing. Those children remain covered by the EUA first granted to remdesivir on May 1 for use in hospitalized patients with severe COVID-19, and expanded on August 28 to include treating all hospitalized patients with COVID-19.
President Donald Trump’s doctors included the drug among his treatments for COVID-19 during his recent hospitalization. Trump took the five-day course. Remdesivir is typically given in treatment courses of five or 10 days, during which patients are dosed intravenously at 200 mg on day 1 followed by 100 mg the other days.
The FDA expanded the EUA for remdesivir following positive results from the Phase III SIMPLE trial which evaluated remdesivir in hospitalized patients with moderate COVID-19 pneumonia (NCT04292730), as well as results from the NIH’s National Institute of Allergy and Infectious Diseases (NIAID) Phase III Adaptive COVID-19 Treatment Trial 1 (ACTT-1; NCT04280705) in hospitalized patients with a range of disease severity.
In ACTT-1, a 1,062-patient study completed September 25, a 10-day course of remdesivir was reported to be superior to placebo in treating hospitalized patients with COVID-19. In data published in The New England Journal of Medicine, patients who were treated with remdesivir showed a 33% faster median time to recovery compared with those who received placebo (10 days compared with 15 days).
“Benefit was most apparent in patients with a baseline ordinal score of 5 (requiring oxygen), a finding most likely due to the larger sample size in this category,” the ACTT-1 researchers wrote.
Kaplan-Meier estimates of mortality by 14 days were 7.1% with remdesivir and 11.9% with placebo.
“Hopeful this lowers the death rate and may potentially reduce LOS [length of stay] days for hospitals. Freeing them up to help those whose healthcare was put on hold.. and hopefully to regain some financially stability sooner rather [than] later,” tweeted Letitia Green, MBA, MEd, Managing Partner and Co-Founder of the Virginia Active Angel Network, LLC (VAAN) and Virginia Investment Capital Group.
Keeping It SIMPLE
SIMPLE was a Phase III randomized trial evaluating the safety and antiviral activity of five-day and 10-day remdesivir regimens compared to standard of care in hospitalized patients with moderate COVID-19. The trial was completed July 27 with an actual enrollment of 1,113 participants.
In August, Gilead researchers published data from the SIMPLE trial in JAMA showing that 584 patients hospitalized with moderate COVID-19, 197 who were randomized to a 10-day course of remdesivir did not have a statistically significant difference in clinical status compared with the 200 who received standard care at 11 days after the start of treatment. The 199 patients randomized to a five-day course of remdesivir had a statistically significant difference in clinical status compared with standard care, but the difference was of uncertain clinical importance, researchers concluded.
The SIMPLE and ACTT-1 trials were two of three Phase III clinical trials upon which the FDA said it based its approval of remdesivir. The other was the SIMPLE-Severe trial (NCT04292899), a randomized, open-label multi-center clinical trial completed July 27 with an enrollment of 4,891 participants.
SIMPLE-Severe assessed the safety and antiviral activity of five-day and 10-day remdesivir regimens compared to standard of care in hospitalized participants with severe COVID-19. Researchers found similar odds of improvement of COVID-19 symptoms in both treatment courses, with no statistically significant differences in recovery rates or mortality rates between the groups.
Remdesivir is a broad-spectrum antiviral adenosine nucleotide prodrug initially developed to treat Ebola. Remdesivir is one of 19 “front runners” among more than 300 COVID-19 drug and vaccine candidates on GEN’s COVID-19 Drug & Vaccine Tracker.
“Today’s approval is supported by data from multiple clinical trials that the agency has rigorously assessed and represents an important scientific milestone in the COVID-19 pandemic,” FDA commissioner Stephen M. Hahn, MD, said in an agency statement. “The FDA is committed to expediting the development and availability of COVID-19 treatments during this unprecedented public health emergency.”
“As soon as possible”
Hahn added that through its Coronavirus Treatment Acceleration Program, the FDA will continue to help move new drugs and vaccines to patients “as soon as possible, while at the same time determining whether they are effective and if their benefits outweigh their risks.”
In its approval letter to Gilead, the FDA through John Farley, MD, MPH, director of the Office of Infectious Diseases, told the company that remdesivir was not referred to an advisory committee for a recommendation on approval “because the application did not raise significant safety or efficacy issues that were unexpected for the drug in the intended population and did not raise significant public health questions on the role of the drug in the diagnosis, cure, mitigation, treatment, or prevention of a disease.”
Hahn and other officials have repeatedly denied that the FDA’s speedy reviews on new COVID-19 drugs and vaccines represented bowing to political pressure from Trump, who has defended his administration’s response to the pandemic and repeatedly pressed the FDA for quick decisions.
On August 22, Trump called out Hahn by his Twitter handle @SteveFDA in a tweet: “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd. Must focus on speed, and saving lives!”
Chinese researchers were first to recommend that the antiviral drug candidate remdesivir and the antimalarial drug chloroquine be assessed in humans as potential treatments for SARS-CoV-2. They based their conclusion on findings showing that “Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro,” the title of a study published as a letter to the editor of the Nature-owned journal Cell Research.
A day later, remdesivir began its first COVID-19 clinical trials in hospitalized patients in Wuhan, China. They included what grew into the first randomized, double-blind, placebo-controlled Phase III trial (NCT04257656) assessing remdesivir in adults admitted to hospital with severe COVID-19. The results, published April 29 in The Lancet, showed that remdesivir failed to show clinical improvement in severely infected patients. In that study, “Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial,” remdesivir had not reduced the presence of SARS-CoV-2 in the bloodstream of 158 patients treated with the antiviral candidate in the 237-patient trial.
“How can Remdesivir get a full @US_FDA approval when there are such mixed data? Not supportive of this decision at all,” tweeted Eric Topol, MD, founder and director of the Scripps Research Translational Institute. “Does it work early? Does it work late? Does it work anytime? So much unresolved.”
Nine late-stage trials
In the United States, remdesivir advanced to Phase III in July, and is now under study in nine late-stage trials that have recruited more than 13,500 patients. In addition to the ACTT-1, SIMPLE, and SIMPLE-Severe trials, remdesivir has also been assessed in six other studies:
- A Phase III randomized, double-blind, placebo-controlled trial (NCT04501952) designed to assess remdesivir’s safety and efficacy in reducing the rate of hospitalization or death in outpatients with early-stage COVID-19, set to enroll up to 1,230 participants.
- The Phase III Adaptive COVID-19 Treatment Trial 2 (ACTT-2; NCT04401579), a NIAID-sponsored trial similar to ACTT-1 except that it is comparing the combination of remdesivir and Eli Lilly’s Olumiant®(baricitinib) to remdesivir alone in hospitalized adults. Currently, 1,034 participants are enrolled.
- The Phase III Adaptive COVID-19 Treatment Trial 3 (ACTT-3; NCT04492475), another NIAID-sponsored trial similar to ACTT-1 and ACTT-2, but comparing the combination of interferon beta-1a and remdesivir to remdesivir alone in hospitalized adults. The trial has an estimated enrollment of up to 1,034 participants.
- The Phase III DisCoVeRy trial (2020-000936-23and NCT04315948), sponsored by the French Institut National de la Santé et de la Recherche Médicale (INSERM). The multi-center, adaptive, randomized, open trial is comparing remdesivir to AbbVie’s Kaletra, Merck KGaA’s Rebif (interferon-beta-1a), and Sanofi’s Plaquenil (hydroxychloroquine) in hospitalized adults with COVID-19. DisCoVeRy has an estimated enrollment of 3,100 participants.
- The Phase II/III CARAVAN trial (NCT04431453), a single-arm, open-label study evaluating the safety, tolerability, and pharmacokinetics (PK) of remdesivir in pediatric participants aged 0 days to < 18 years with COVID-19. The trial has an estimated enrollment of 52 participants.
- The Phase III World Health Organization (WHO) Solidarity Trial comparing remdesivir and AbbVie’s Kaletra®(lopinavir/ritonavir) plus interferon beta-1a to standard of care in hospitalized patients with COVID-19. The trial has recruited 11,266 patients worldwide. In July, the WHO halted Solidarity’s study of hydroxychloroquine and Kaletra alone after interim results showed they did not reduce mortality.
Billions in Projected Sales
Annual sales projections for remdesivir have pegged the drug as generating a number in the low billions of dollars. In June, Geoffrey C. Porges, MBBS, director of therapeutics research and a senior research analyst at SVB Leerink, projected $2 billion in sales for remdesivir this year, climbing to $7.7 billion by 2022.
However, Jefferies managing director Michael Yee projected between $1 billion and $3 billion this year, after Gilead raised its sales forecast for 2020 to between $23 billion and $25 billion after the second quarter, from its earlier guidance of between $21.8 billion and $22.2 billion.
Morningstar analyst Karen Andersen, CFA, one of GEN’s “ Ten Life Science Analysts to Watch in 2020,” projected in September that remdesivir could generate $3 billion in 2021 sales.
Failing, then Prequalifying, Remdesivir
Just last week, researchers working with the WHO posted interim results from the Solidarity trial which included remdesivir among four antiviral treatments that they said failed to show effectiveness in hospital inpatients with COVID-19.
“Remdesivir, hydroxychloroquine, lopinavir [co-administered with ritonavir] and interferon regimens appeared to have little or no effect on hospitalized COVID-19,” the researchers concluded in a preprint posted in medRxiv on October 15.
At least one analyst worried at the time that the disappointing results from Solidarity could hinder Gilead’s prospects of FDA approval for remdesivir–a scenario that the FDA put to bed with its full authorization for the drug: “Although the FDA probably doesn’t have it in them to pull an EUA, this could jeopardize full approval,” wrote Brian P. Skorney, CFA, Senior Research Analyst with Baird.
Skorney added: “We believe it will certainly see a limitation of use, especially outside the U.S.”
The same day the Solidarity results were posted, the WHO added the antiviral drug to its “prequalified” list, supporting its use by the UN and other global entities. Remdesivir became the 579th medicine or finished pharmaceutical product—and the first COVID-19 therapeutic—to receive prequalified status from the WHO. The WHO prequalifies drugs whose manufacturers have shown the agency that they have the capacity to produce a product of consistent quality in accordance with international standards and WHO/UNFPA-United Nations Population Fund specifications.
“The speed and rigor with which Veklury has been developed and approved in the United States reflect the shared commitment of Gilead, government agencies, and clinical trial investigators to advance well-tolerated, effective treatment options for the fight against COVID-19,” Gilead’s O’Day added. “We will continue to work at speed with the aim of enhancing patient outcomes with Veklury to ensure all patients with COVID-19 have the best chance at recovery.”