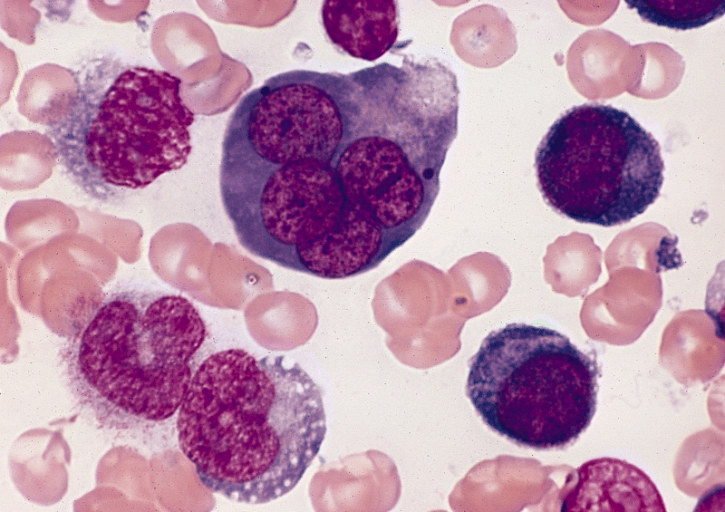
Acute erythroid leukemia (AEL) is a high-risk cancer with a dismal prognosis, uncertain genetic basis, and controversy surrounding the diagnosis, according to researchers. That is changing, thanks to research led by St. Jude Children’s Research Hospital that appears today in the journal Nature Genetics.
Now, a team led by St. Jude Children’s Research Hospital reports the completion of what they say is the largest, most comprehensive genomic analysis yet of AEL and identified six age-related subgroups with distinct mutations and patterns of gene expression as well as treatment outcomes. The analysis (“Genomic subtyping and therapeutic targeting of acute erythroleukemia”), which appears in Nature Genetics, revealed that 45% of patients had mutations in signaling pathways that help drive uncontrolled cell growth. Researchers also reported evidence that the leukemia may be vulnerable to existing precision medicines.
“…AEL is a high-risk leukemia of poorly understood genetic basis, with controversy regarding diagnosis in the spectrum of myelodysplasia and myeloid leukemia. We compared genomic features of 159 childhood and adult AEL cases with non-AEL myeloid disorders and defined five age-related subgroups with distinct transcriptional profiles: adult, TP53 mutated; NPM1 mutated; KMT2A mutated/rearranged; adult, DDX41 mutated; and pediatric, NUP98 rearranged. Genomic features influenced outcome, with NPM1 mutations and HOXB9 overexpression being associated with a favorable prognosis and TP53, FLT3, or RB1 alterations associated with poor survival. Targetable signaling mutations were present in 45% of cases and included recurrent mutations of ALK and NTRK1, the latter of which drives erythroid leukemogenesis sensitive to TRK inhibition,” the investigators wrote.
“This genomic landscape of AEL provides the framework for accurate diagnosis and risk stratification of this disease, and the rationale for testing targeted therapies in this high-risk leukemia.”
“Genomic alterations and gene expression profiles were the strongest predictors of outcome in patients with AEL, which suggests they should be incorporated into the diagnostic and prognostic criteria,” said corresponding author Charles Mullighan, MD, a member of the St. Jude department of pathology. “These results mark a new era in understanding and treatment of AEL, an aggressive leukemia that has been plagued by diagnostic controversy and poor outcomes.”
AEL is a rare subtype of acute myeloid leukemia that is more common in adults than children. AEL is often unresponsive to conventional therapy and overall long-term survival is less than 10%.
Classifying AEL in the spectrum of myeloid leukemia has been a challenge since the leukemia was first described almost a century ago. The diagnostic criteria have changed over the decades, most recently in 2016, but the genomic basis of AEL remained uncertain. As a result, in 2016 some cases once defined as AEL were reclassified as AML or myelodysplastic syndrome (MDS). AEL, AML, and MDS are all myeloid cancers, or cancer of bone marrow cells, but require different treatments of significantly different intensity.
Researchers in this study compared the mutational landscape of 159 children and adults diagnosed with AEL to 1,903 patients with non-AEL myeloid disorders, including AML and MDS. The analysis included the whole genome, whole exome, or whole transcriptome sequencing data. The patients were from the U.S., Europe, Singapore, Japan, and Australia. They ranged from infants to adults age 60 and older.
“We found that patients with AEL, AML, and MDS had many of the same mutations, but the frequency and patterns of the mutations were very different,” said first author Ilaria Iacobucci, PhD, a scientist in the Mullighan laboratory. “The findings demonstrate AEL is a specific subtype and offer insights into how the disease process and outcomes vary in children and adults.”
For example, alterations in one or both copies of the tumor suppressor gene TP53 were a hallmark of an AEL subset that occurred almost exclusively in older adults. The subset accounted for 32% of the cases in this analysis and was associated with a dismal prognosis. There were no long-term survivors.
In contrast, about 12% of adult patients were in a subgroup defined by mutations in the NPM1 gene and had a good prognosis. More than 87% of patients were long-term survivors.
“Identifying the genomic basis of AEL also led to the identification of novel treatment targets in signaling pathways and early evidence of effectiveness,” said co-author Torsten Haferlach, MD, of the MLL Munich Leukemia Laboratory. Kinases help regulate gene activity and are frequently mutated in cancer.
For example, a mouse model of AEL that included mutations in TP53 and NTRK1, a kinase in a signaling pathway, was exquisitely sensitive to the inhibitor larotrectinib. AEL remained undetectable in the mice for at least three months following treatment.
“The results highlight a potential role for such inhibitors in future clinical trials,” Mullighan said.