An international research team headed by scientists in France has used gene therapy to restore hearing in adult mice with DFNB9 deafness, one of the most common forms of hereditary, or congenital deafness. As well as preventing hearing loss when administered to the developing cochlea in young mice, the gene therapy approach—in which separate viral vectors are used to deliver the protein otoferlin as two halves—also reversed deafness in adult DFNB9 mice.
The scientists say their achievement could pave the way to human gene therapy trials in patients with DFNB9 deafness. “Our results document both the preventive and curative efficacies of local gene therapy in a mouse model of DFNB9, while expanding the scope of potential AAV gene therapy applications for human hereditary deafness forms,” they wrote in their published paper in PNAS, which is titled, “Dual AAV-mediated gene therapy restores hearing in a DFNB9 mouse model.” The team comprised collaborating researchers at The Institut Pasteur, Inserm, CNRS, Collège de France, Sorbonne University, the University of Clermont Auvergne in France, together with colleagues at the University of Florida, Gainesville, Columbia University Medical Center, and New York Presbyterian Hospital in the U.S.
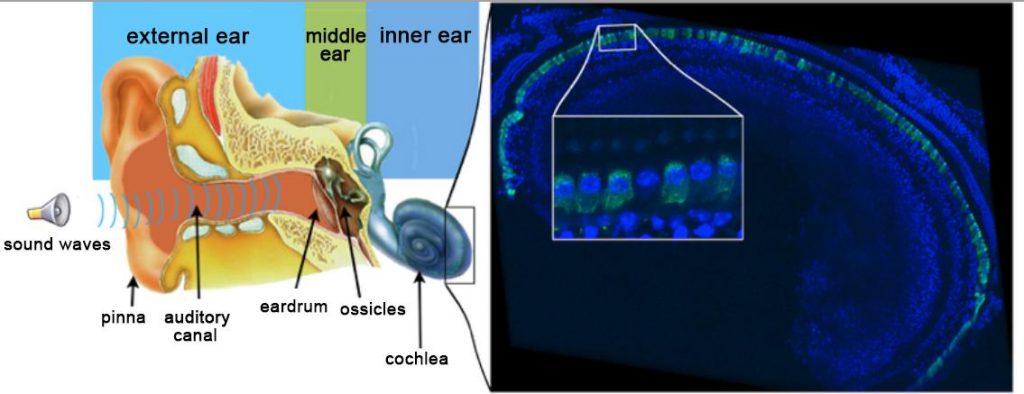
Autosomal recessive genetic forms of deafness account for most cases of profound hearing loss, the researchers wrote. “More than half the cases of nonsyndromic profound congenital deafness have a genetic cause, and most (∼80%) are autosomal recessive (DFNB).” Cochlear implants are currently the only treatment option, and while they can help improve hearing, they are not perfect. Patients will still commonly have problems discerning speech in noisy environments, or music, for example.
Adeno-associated viruses (AAV) are showing promise as vectors for gene delivery in gene therapy, and could feasibly be used to deliver the genes needed to restore hearing in congenital forms of deafness. Sustained transgene expression with AAVs has been achieved in various animal models, and the excellent safety profile of these vectors has been demonstrated in many ongoing clinical trials,” the authors noted. “As a result, AAVs are now the principal gene delivery system used in gene therapy for genetic disorders.”
However, in most tests in mouse models of deafness, the required gene has been administered to the developing cochlea in newborn mice (usually about postnatal day 1 or 2—P1 or P2), which is before the animals start to be able to hear, at about P12. In contrast, in humans cochlear development is completed in the fetus during pregnancy and hearing is possible by about 20 weeks gestation, well before birth. This results in a very small therapeutic window if gene therapy is to be carried out in the developing cochlear. In reality, gene therapy would have to be administered after birth, once the hearing loss and its cause have been diagnosed in the young infant, and after the cochlea is fully developed. This means treatment must be able to reverse pre-existing deafness, and this should be taken into account when devising preclinical tests.
The potential use of AAV technology to deliver the otoferlin gene should be hampered by the limited DNA packing capacity of AAV vectors—about 4.7 kb of DNA—which would not be enough to carry the complete recombinant otoferlin gene, which is about 6 kb. Saffiedine’s team devised a way around this that used a dual AAV-vector approach, in which the otoferlin gene is effectively split between two different AAV vectors, with each encoding one of the two opposite ends of the otoferlin gene.
The team first simultaneously administered the two vectors directly into the cochleas of DFNB9 mice that lack the otoferlin gene, at postnatal day 10 (P10). This is before cochlear development is completed. Analysis of the cochlear tissue eight weeks after the single injection of both vectors confirmed that the treatment resulted in production of the complete otoferlin protein in more than 60% of the IHCs. Auditory brainstem response tests 4 weeks after gene delivery confirmed that the animals’ hearing was restored, and this hearing regain was still evident in most of the mice more than 6 months later. “Thirty weeks after the injection, six of the eight mice receiving injections on P10 still had hearing thresholds within 10 dB of those of wild-type mice,” the authors wrote. “Gene therapy before hearing onset therefore prevents deafness in Otof–/– mice.
Encouragingly, tests in mice receiving a single intracochlear injection of the vector pair at either P17 or P30 showed that the treatment resulted in otoferlin production in IHCs throughout the treated cochlea, and resulted in hearing restoration as early as 3 weeks post-injection, up to 20 weeks, when the animals were tested again.
“We report here, in the DFNB9 mouse model, our proof of principle that cochlear delivery of a fragmented cDNA via a dual-AAV vector approach can effectively restore production of the full-length protein, resulting in a long-lasting correction of the profound deafness phenotype of these mice,” the authors concluded. “We show that local gene therapy in the mutant mice not only prevents deafness when administered to immature hearing organs, but also durably restores hearing when administered at a mature stage, raising hopes for future gene therapy trials in DFNB9 patients.” The findings also indicate that the therapeutic window for gene therapy against DFNB9 deafness may be longer than previously thought, “raising hopes for future gene therapy trials in DFNB9 patients.”


