Much of the current research on the gut microbiome focuses on the collection of bacteria that reside within collective communities. Yet these microbes represent only one fraction of the gut microbiota, which holds communities of viruses, protists, archaea, and fungi—which have been largely overlooked. However, a team of investigators at the University of Alabama at Birmingham (UAB) and University of Tennessee Health Science Center is looking to change that by focusing on the communities of molds and yeasts in the intestine, called the mycobiome. In a new study on mice, the researchers show a significant role for fungi in shaping metabolism for various host diets. Findings from the study were published recently in Communications Biology through an article titled, “The gut mycobiome of healthy mice is shaped by the environment and correlates with metabolic outcomes in response to diet.”
“We showed that the gut mycobiome of healthy mice is shaped by the environment, including diet, and significantly correlates with metabolic outcomes, explained co-senior study investigator Kent Willis, MD, an assistant professor at UAB. “Our results support a role for the gut mycobiome in host metabolic adaptation, and these results have important implications regarding the design of microbiome studies and the reproducibility of experimental studies of host metabolism.”
The UAB team looked at fungi in the jejunum of the mouse small intestine, the site of the most diverse fungal population in the mouse gut. They found that exposure to a processed diet, which is representative of a typical Western diet rich in purified carbohydrates, led to persistent differences in fungal communities that significantly associated with differential deposition of body mass in male mice, as compared to mice fed a standardized diet.
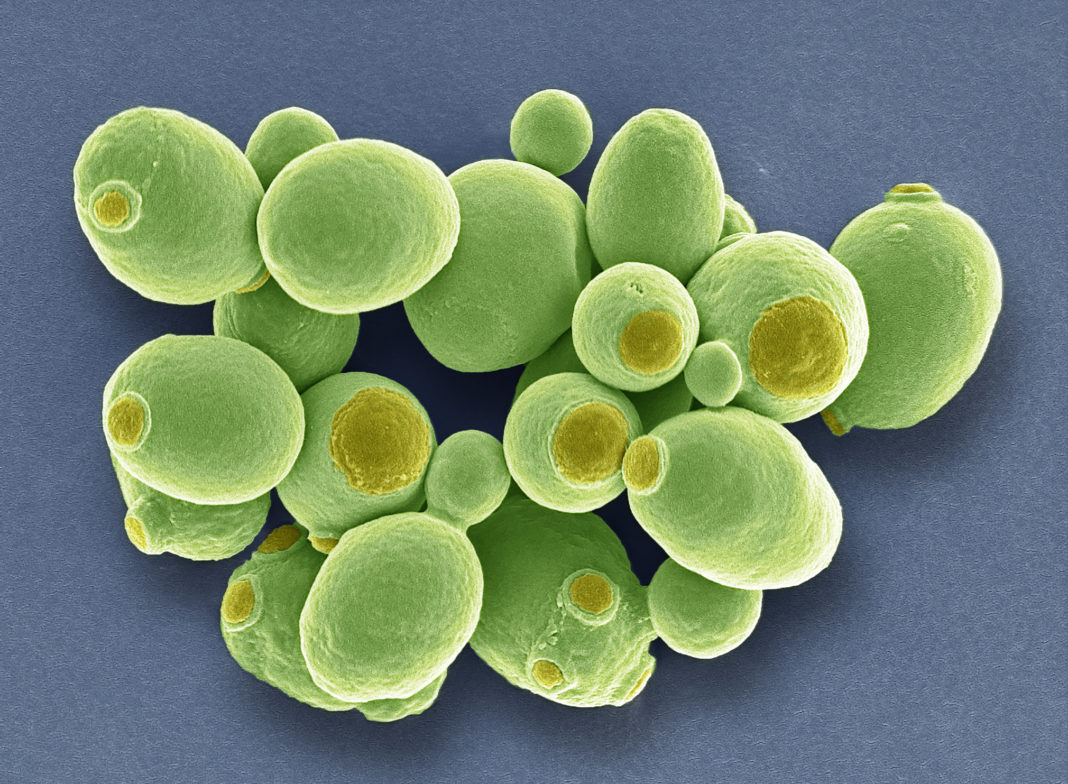
“We demonstrated that exposure to processed diet leads to persistent differences in fungal communities that significantly associate with differential deposition of body mass in male mice compared to mice fed standardized diet,” the authors wrote. “Fat deposition in the liver, transcriptional adaptation of metabolically active tissues, and serum metabolic biomarker levels are linked with alterations in fungal community diversity and composition. Specifically, variation in fungi from the genera Thermomyces and Saccharomyces most strongly associated with metabolic disturbance and weight gain.”
Interestingly, the study had an ingenious starting point. The researchers obtained genetically identical mice from four different research animal vendors. It is known that gut bacterial communities vary markedly by the vendor. Similarly, the researchers found dramatically different variability by the vendor for the jejunum mycobiomes, as measured by sequencing internally transcribed spacer rRNA. At baseline, mice from one of the vendors had five unique fungal genera, and mice from the other three vendors had three, two, and one unique genera, respectively.
They also looked at interkingdom community composition—meaning bacteria as well as fungi—and found large baseline bacterial community differences. From this initial fungal and bacterial diversity, they then measured the effects of time and differences in diet—standardized chow versus the highly processed diet—on fungal and bacterial community composition.
The researchers also addressed a fundamental question: Are the fungal organisms detected by next-generation sequencing coming from the diet, or are they true commensal organisms that colonize and replicate in the gut? They compared sequencing of the food pellets, which contained some fungi, and the contents of the mouse jejunum to show the jejunum fungi were true commensal colonizers.
Thus, this study showed that variations in the relative abundance and composition of the gut mycobiome correlate with key features of host metabolism. This lays a foundation towards understanding the complex interkingdom interactions between bacteria and fungi and how they both collectively shape and potentially contribute to host homeostasis.
“Our results highlight the potential importance of the gut mycobiome in health, and they have implications for human and experimental metabolic studies,” concluded co-senior study investigator Joseph Pierre, PhD, assistant professor at the University of Tennessee Health Science Center. “The implication for human microbiome studies, which often examine only bacteria and sample only fecal communities, is that the mycobiome may have unappreciated effects on microbiome-associated outcomes.”