Asthma is the most common chronic condition in children and affects nearly one in ten children in developed countries. A respiratory virus is one of the most common causes of asthma symptoms in children five years old and younger. However, the cause of asthma is still unknown. If a child has a family history of asthma or allergies, they have a higher chance of getting asthma early in life. Now, new research finds that an overgrowth of yeast in the gut within the first few months of life may cause changes to the immune system which increases asthma risk later on.
The findings were published in the journal eLife in a paper titled, “Bacterial-fungal interactions in the neonatal gut influence asthma outcomes later in life,” and led by researchers at the University of British Columbia. Their findings may explain a potential cause of asthma and may lead to new studies to prevent this chronic condition.
“Bacterial members of the infant gut microbiota and bacterial-derived short-chain fatty acids (SCFAs) have been shown to be protective against childhood asthma, but a role for the fungal microbiota in asthma etiology remains poorly defined,” wrote the researchers.
The gut microbiome influences immunological, endocrine, and neural pathways and plays an important role in infant development. The window after birth is a critical time for the development of a healthy immune system and gut microbiome.
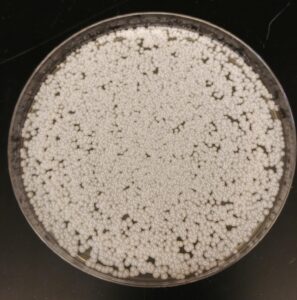
The researchers began with a study of 123 newborns in Canada, who were part of the CHILD Cohort Study. They observed an overgrowth of P. kudriavzevii in the stools of the newborns during the first three months of life was associated with a higher risk of asthma.
The researchers then applied P. kudriavzevii to newborn mice with immature gut microbiota communities. The team discovered that the newborns exposed to the yeast experienced more lung inflammation than those who were unexposed. However, P. kudriavzevii in an adolescent mouse model did not cause this excess inflammation.
“Our findings show that there is a critical window in early life where disruptions in the gut microbiota caused by P. kudriavzevii affect the development of the immune system and increase the risk and severity of asthma later in life,” Boutin said.
“We further show that P. kudriavzevii growth and adherence to gut epithelial cells are altered by SCFAs,” noted the researchers. “Collectively, our results underscore the potential for leveraging inter-kingdom interactions when designing putative microbiota-based asthma therapeutics.”
Their study may lead to potential future studies that further expand on studying P. kudriavzevii‘s link to asthma risk in early development.
“Immune responses to gut microbe disruptions early in life have long-term consequences for diseases of the immune system later in life,” concluded senior author Brett Finlay, PhD, professor at the Michael Smith Laboratories and the departments of biochemistry and molecular biology, and microbiology and immunology, University of British Columbia. “Our study adds to our understanding of microbiota-associated asthma and suggests that inhibiting yeast overgrowth with SCFAs in early life could be an effective approach to preventing this condition.”



