Researchers in Switzerland suggest that helping the brain to flush out toxic proteins could represent a new approach to preventing or treating age-related neurological disorders such as Alzheimer’s disease. Studies in mice by the team based at ETH Zurich and the University of Zurich have shown for the first time that the lymphatic system plays a key role in draining the cerebrospinal fluid (CSF) that bathes the brain, but that this function slows with age.
“Our findings implicate that the lymphatic system has a greater than previously acknowledged role in many neurological conditions,” the researchers write in their published paper in Nature Communications (“Outflow of Cerebrospinal Fluid Is Predominantly through Lymphatic Vessels and Is Reduced in Aged Mice”). “If so, the lymphatic system may represent a possible new therapeutic target with the aim to enhance the clearance of toxic proteins from the CSF and the brain.”
About half a liter of CSF is produced in the cerebral ventricles every day, which also has to be cleared from the cranial cavity. Scientists know that CSF can be drained from the brain via two potential exit routes—the blood vessels and the lymphatic vessels—and it has previously been assumed that the venous system represents the primary clearance pathway. A team headed by Michael Detmar, M.D., professor of pharmacogenomics at ETH Zurich, and Steven Proulx, Ph.D., has now turned this assumption on its head, and identified the lymphatic system as the major route for CSF drainage.
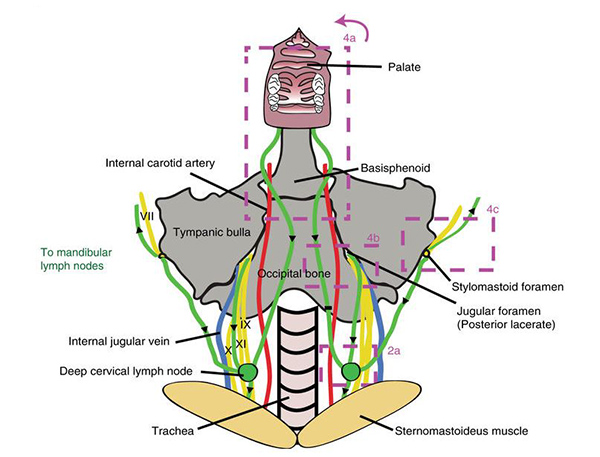
The team had previously developed near-infrared (NIR) tracers that can be used to image the lymphatic system but which, unlike other tracers, don’t stick to tissue components, aren’t taken up directly by blood vessels, and are not phagocytosed by macrophages. The team injected these fluorescent dye molecules into mouse brain ventricles and then tracked the dye-spiked CSF as it passed into the peripheral blood vessels and the lymphatic vessels directly draining the skull.
The imaging results showed how the CSF exited the skull along cranial nerve sheaths, primarily those around the olfactory and optic nerves, and within just a few minutes appeared in the lymphatic vessels and lymph nodes external to the brain. Surprisingly, however, no dye reached the blood vessels in the same time period. It took much longer for any dye to reach the veins, and the imaging studies indicated that the CSF drains into the lymph vessels and then into the venous system. “On the basis of our dynamic imaging data, we conclude that lymph transport was the main route for tracer movement from the CSF into the systemic bloodstream rather than direct blood outflow through the posterior facial vein,” they write. “Once in tissue outside the brain, it is removed by the lymphatic vessels,” confirms Qiaoli Ma, a doctoral student in Detmar's group and lead study author.
The scientists next applied a technique they developed using a specific tracer, P40D680, to quantify lymphatic outflow of CSF in both young, and old mice. They found that CSF outflow was much slower in the older mice than in the young animals, possibly because less CSF is produced. “To our knowledge, our study is the first to demonstrate a reduction of lymphatic outflow of CSF with aging,” the authors write.
This finding has particular significance because the brain isn’t well served by the body’s immune system and instead relies on clearance of CSF to remove unwanted toxins. “The immune system eliminates toxins elsewhere in the body, but the brain is considered to be largely disconnected from this system,” Proulx states. “Only a few immune cells have access under normal conditions. The CSF steps into the breach here. By constantly circulating, it flushes the brain and removes unwanted substances.”
The slowing of CSF clearance in the brains of aging mice could therefore have implications for the study and potentially treatment of neurological disorders such as Alzheimer’s disease, which is caused by an accumulation of misfolded protein in the brain. The scientists suggest that it may feasibly be possible to help clear these toxic proteins from the brain using drugs that boost lymphatic flow. They hope to investigate whether stimulating CSF flow could slow down the development of dementia in mice. “Although demonstration of this phenomenon in humans still awaits, this study sets the stage for investigation of a potentially important role for the lymphatic system in a multitude of CNS-related pathologies,” they suggest. Other avenues of potential research include investigating whether lymphatic flow might impact on inflammatory diseases of the central nervous system, such as multiple sclerosis.
“On the basis of our dynamic imaging data, we conclude that lymph transport was the main route for tracer movement from the CSF into the systemic bloodstream rather than direct blood outflow through the posterior facial vein,” the team concludes. “A significant decline in CSF lymphatic outflow is found in aged compared to young mice, suggesting that the lymphatic system may represent a target for age-associated neurological conditions.”