![During mitosis, a cell’s chromosomes (blue) rapidly divide. When telomeres (green) are no longer protected by the protein TRF2, the cell receives a signal to undergo cell death (red). [Salk Institute]](https://genengnews.com/wp-content/uploads/2018/08/June25_2015_SalkInst_TelomereDeprotection1767621132-1.jpg)
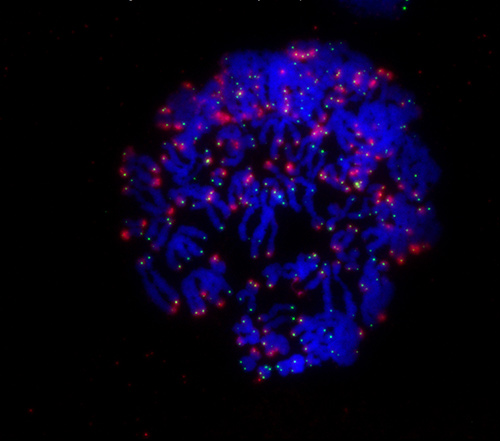
During mitosis, a cell’s chromosomes (blue) rapidly divide. When telomeres (green) are no longer protected by the protein TRF2, the cell receives a signal to undergo cell death (red). [Salk Institute]
Cancer cells of many types are known to avoid crisis, the mechanism that culminates in cell death. But what if these cancer cells could be nudged back to crisis? Inducing cancer cells to self-destruct would open new therapeutic possibilities, not the least of which would be the development of enhanced forms of chemotherapy.
To bring these possibilities closer to realization, researchers centered at the Salk Institute decided to reexamine cell death during crisis, the details of which remained sketchy. These researchers, led by Jan Karlseder, Ph.D., found that telomeres played a larger role in the cell’s self-destruct mechanism than was previously appreciated.
The research team knew from previous work that during artificially lengthened mitosis, telomeres are deprived of the protective effects of a protein that essentially keeps them clear of the cell’s self-destruct mechanism. Without the benefit of this protein, telomeres are identified as damaged DNA, and crisis ensues.
In its new work, the researchers found that the same kind of deprotection can occur even if mitosis is not artificially lengthened. They did real-time imaging of cells in a dish to track the cells' fate through one or more mitotic cycles, and they found that a type of cellular stress called telomere fusion could evoke a prolonged mitosis and eventually crisis. Cells in this state lost their telomere-protecting protein and activated the self-destruct sequence.
“There was a long-standing hypothesis that turned out to be incorrect: that cells simply start to fuse chromosomes and break apart, generating instability and cell death,” said Dr. Karlseder. “What we show instead is it a much more targeted pathway that really only takes one cell cycle to cause crisis—it has nothing to do with the slow and steady accumulation of genomic instability.”
The new findings appeared June 24 in Nature, in an article entitled, “Cell death during crisis is mediated by mitotic telomere deprotection.”
“[Human] cells in crisis undergo spontaneous mitotic arrest, resulting in death during mitosis or in the following cell cycle. This phenotype is induced by loss of p53 function, and is suppressed by telomerase overexpression,” wrote the authors. “Telomere fusions triggered mitotic arrest in p53-compromised non-crisis cells, indicating that such fusions are the underlying cause of cell death.”
The authors added that by exacerbating mitotic telomere deprotection, they could increase the ratio of cells that died during mitotic arrest and sensitize cancer cells to mitotic poisons.
Anthony Cesare, Ph.D., a researcher at Children's Medical Research Institute in Australia and a contributor to the work, said the finding was very exciting and that it was unexpected to see how events early in the cell cycle, telomere fusions, are passed to a later stage of the cell cycle, mitosis. “This opens up new avenues for understanding how telomeres control cell growth and the implications of telomere biology in chemotherapy,” he noted.
Several chemotherapies—such as Taxol for breast cancer—seek to stop cancer by interrupting mitosis so cancer cells can no longer divide. The researchers hypothesize that they can enhance these mitotic inhibitors by, for example, deprotecting telomeres first to make the cells more susceptible to drugs. It might also be possible to see if cells from a particular tumor had shorter or deprotected telomeres and, if so, expect that tumor to be much more sensitive to mitotic inhibitors.
“The pathway we've found challenges a long-held hypothesis on cellular behavior during early tumor formation,” explained Makoto Hayashi, Ph.D., a researcher at Kyoto University and first author of the new work. “Comprehensive understanding of the pathway will hopefully provide us a novel method of early tumor diagnosis and a therapeutic opportunity for very early stage of cancer.”