Scientists from the Washington University School of Medicine in St. Louis report that mice missing two important proteins of the vascular system develop normally and appear healthy in adulthood, as long as they don't become injured. If they do, their wounds don't heal properly, note the researchers, who add that their work may have implications for treating diseases involving abnormal blood vessel growth, such as the impaired wound healing often seen in diabetes and the loss of vision caused by macular degeneration.
Their study (“Endothelial cell FGF signaling is required for injury response but not for vascular homeostasis”) appears in the Proceedings of the National Academy of Sciences online early edition.
The paper's senior author, David M. Ornitz, M.D., Ph.D., the Alumni Endowed Professor of Developmental Biology, studies fibroblast growth factors (FGFs), which are signaling molecules that play broad roles in embryonic development, tissue maintenance, and wound healing. They interact with specific receptor molecules, FGFRs, located on the surface of many types of cells in the body.
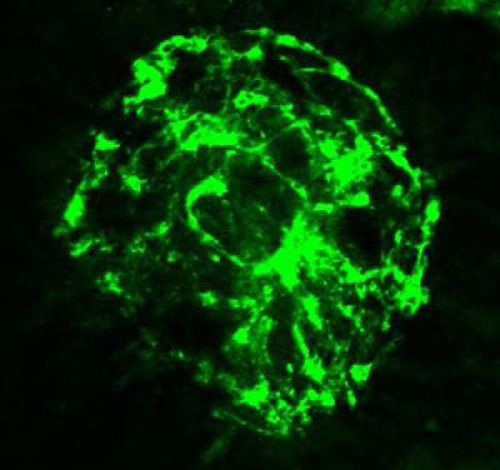
When an organ is injured, the healing process involves the growth of new blood vessels. Since the cells lining the interior of blood vessels and blood cells themselves are important for developing new vasculature, Dr. Ornitz and his colleagues asked what would happen if they turned off signaling of the FGFR1 and FGFR2 proteins, two major mediators of the FGF signal that are present in the cells that line blood vessels. Their strategy differed from past studies, which shut down this signaling more broadly.
“The first thing we noticed, and we were rather surprised by this, was that the mice were completely normal,” said Dr. Ornitz. “They were running around and lived to a ripe old age. We did genetic tests to make sure they actually lacked these proteins. But when we challenged these mice, we saw that they healed from a skin injury more slowly than their normal littermates, and we found that the density of blood vessels surrounding the injury site was significantly decreased.”
With collaborator and co-senior author Rajendra S. Apte, M.D., Ph.D,. the Paul A. Cibis Distinguished Professor of Ophthalmology and Visual Sciences, the researchers also looked at the eyes. Like any other organ, new blood vessels grow in the eye in response to disease or injury. But unlike the rest of the body, new blood vessels are not desired here, since they bleed, cause scar tissue formation, and block light to the retina, causing vision loss.
The new work suggests that increasing FGF signaling in the body might help improve wound healing by increasing new blood vessel growth following an injury, especially in those who have trouble healing, such as patients with diabetes-related foot ulcers. Dr. Ornitz pointed out that human FGF2 is already in clinical use as a topical spray in Japan for foot ulcers and similar wound healing purposes.
Conversely, inhibiting these pathways in the eye might help patients with age-related macular degeneration or diabetic retinopathy. Such patients grow new blood vessels in response to these diseased or injured states, but the new vessels only serve to obscure vision, not help heal an abnormal eye. And since the research suggests these FGF pathways are not involved with normal development and tissue maintenance, any treatments boosting or inhibiting these signals would likely not effect healthy tissue.
“That's an important point,” said Dr. Apte, who treats patients at Barnes-Jewish Hospital. “In diabetes, the normal blood vessels of the retina become fragile because the disease affects them. With any targeted therapy, we worry about damaging the normal vessels. But our work suggests that inhibiting FGF signaling in the eye may prevent this abnormal response without harming normal vessels.”