Scientists in Japan have used CRISPR-Cas9 technology to stop human immunodeficiency virus type 1 (HIV-1) replication in latently infected T cells that can’t be controlled using existing drug treatments. The gene-editing approach effectively disrupts two regulatory HIV-1 genes, tat and rev, which are essential for viral replication. Describing their in vitro studies in Scientific Reports, the researchers at Kobe University Graduate School of Medicine and Kobe University Graduate School of Health Sciences say initial results indicate that using CRISPR-Cas9 to target HIV-1 regulatory genes may offer a new approach to achieving “functional cures.”
“These results show that the CRISPR-Cas9 system, by targeting the regulatory genes of HIV-1, tat and rev, is a promising method for treating HIV infection,” comments co-author Masanori Kameoka, Ph.D., an associate professor at Kobe University Graduate School of Health Sciences. “We now need to investigate how we can selectively introduce a CRISPR-Cas9 system that targets HIV-1 genes into the infected cells of patients.”
The team’s published paper, co-authored by Dr. Kameoka, and co-researchers Youdiil Ophinni, Ph.D., Mari Inoue, Ph.D., and Tomohiro Kotaki, Ph.D., is entitled “CRISPR/Cas9 System Targeting Regulatory Genes of HIV-1 Inhibits Viral Replication in Infected T-Cell Cultures.”
HIV-1 infects about 35 million people worldwide, and while lifelong antiretroviral therapy (ART) can help convert what is otherwise a deadly infection into a more “manageable chronic disease,” current treatments are not a cure because they can’t completely eradicate the virus, which inserts its genes into the host cells’ DNA, the authors explain. Despite treatment using ART, HIV-1 continues to replicate at a very low level in some latently infected immune system cell types, such as CD4+ cells, macrophages, and follicular dendritic cells. “Current antiviral compounds are incapable of targeting the integrated proviral genome inside these cellular reservoirs and rapid viral rebound ensues after ART cessation,” they explain. The virus can also hide out in tissues such as the central nervous system.
CD4+ T cells have been the most studied of the cellular reservoirs in which HIV-1 can persist. A small fraction of resting CD4+ T cells will harbor HIV-1, even during ART, and are considered to be “the major obstacle to HIV-1 eradication,” the authors point out. “Latent HIV-1 infection in resting CD4+ T cells is the primary cause of the barrier to a functional cure.” They suggest that a “single-time intervention to clear viral genomic persistence represents a sensible and promising approach to achieve a HIV-1 functional cure.”
One potential approach to eradicating HIV-1 from such reservoirs is to directly disrupt the proviral genome using genome-editing tools. Unfortunately, technologies such as zinc finger nuclease (ZFN) and transcription activator-like effector nuclease (TALEN) have proven problematic because of “difficulties associated with the design, synthesis, and protein validation for a specific gene locus of interest.”
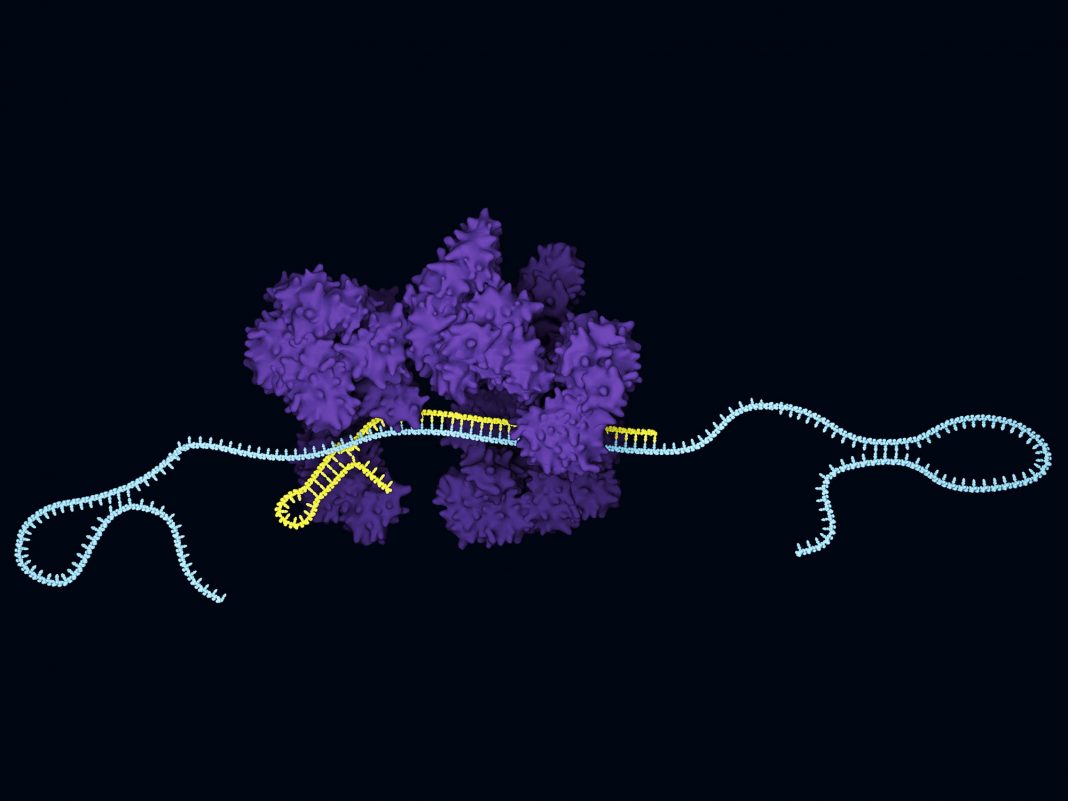
The Kobe University Graduate School team has now developed an alternative approach using CRISPR-Cas9 gene editing to disrupt two regulatory viral genes, tat and rev, which are essential for viral replication, and which are also highly conserved across different HIV-1 subtypes.
The scientists generated six guide RNAs (gRNAs)—three targeting tat and three targeting rev—to direct the DNA-cleaving Cas9 enzyme to the relevant sites in the proviral DNA. They packaged gRNAs and the Cas9 enzyme system into a lentiviral vector, which they could then introduce into cultured cells.
Initial studies demonstrated that the vector effectively abolished expression of tat and rev in cultured cells that were engineered to express the genes. The target genes were mutated at the Cas9 cleavage sites with “high frequency and various indel [insertion/deletion] mutations,” the authors write. Encouragingly CRISPR-Cas9 transduction of human T cells had no effect on cell viability, and there were no detectable off-target mutations in the human DNA.
The CRISPR constructs also targeted tat and rev expression in latently infected CD4+ T cells, “proving that lentiviral delivery of the CRISPR/Cas9 system successfully reached and cleaved the dormant HIV-1 proviral genome,” they state. The constructs also markedly suppressed cytokine-dependent HIV-1 reactivation in latently infected cells and inhibited viral replication in persistently infected cells. The team says these results “demonstrated that the lentiviral delivery of CRISPR/Cas9 successfully reached the isolated proviral genome, cleaved regulatory genes, and significantly inhibited viral replication, even after latency reversal.”
They claim that the ability to transduce nondividing cells, such as resting CD4+ T cells, using lentiviral constructs and achieve long-term Cas9 transgene expression supports the feasibility of using the system to eradicate cells that act as latent reservoirs of HIV-1.
They acknowledge that further research will be needed to translate their early in vitro work into in vivo preclinical models and human patients. “In order to safely and effectively introduce the CRISPR-Cas9 system, the vectors must be improved,” Dr. Kameoka notes. “We hope this research will provide us with useful information in developing a treatment method that can completely cure HIV-1 infection.”
“The capability of lentiviral vectors to transduce non-dividing cells, including resting CD4+ T cells, and maintain stable, long-term Cas9 transgene expression supports their potential use in eradicating infected cells constituting the latent reservoir,” the researchers conclude. “Based on the rapid advances being achieved in CRISPR/Cas9 research, a HIV-1 functional cure may soon be within reach.”