The COVID-19 vaccine landscape has three to four dozen contenders. Multiple companies such as Moderna Therapeutics, Inovio Therapeteutics, Janssen, and Sanofi Pasteur are working on their own hopeful candidates. Academic groups are also pushing forward with firm footing. Indeed, one example comes from an announcement today from scientists at the University of Pittsburgh School of Medicine that their vaccine candidate produces antibodies specific to SARS-CoV-2 in mice, at quantities thought to be sufficient for neutralizing the virus.
Two important characteristics set this vaccine apart. First, the vaccine is delivered through a fingertip-sized patch. Second, the data regarding the vaccine’s efficacy represent the first peer-reviewed study that describes a candidate vaccine for COVID-19.
The paper titled, “Microneedle array delivered recombinant coronavirus vaccines: Immunogenicity and rapid translational development” appears in EBioMedicine.
The researchers were able to act quickly because they had already laid the groundwork during earlier coronavirus epidemics.
“We had previous experience on SARS-CoV in 2003 and MERS-CoV in 2014. These two viruses, which are closely related to SARS-CoV-2, teach us that a particular protein, called a spike protein, is important for inducing immunity against the virus. We knew exactly where to fight this new virus,” said co-senior author Andrea Gambotto, MD, associate professor of surgery at the Pitt School of Medicine. “That’s why it’s important to fund vaccine research. You never know where the next pandemic will come from.”
“Our ability to rapidly develop this vaccine was a result of scientists with expertise in diverse areas of research working together with a common goal,” said co-senior author Louis Falo, MD, PhD, professor and chair of dermatology at Pitt’s School of Medicine.
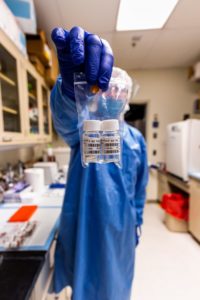
The vaccine described in this paper—called PittCoVacc (short for Pittsburgh Coronavirus Vaccine)—uses lab-made pieces of the spike protein of the virus to build immunity. It’s construction is similar to the seasonal vaccine against the influenza virus.
The researchers also used a novel approach to deliver the drug, called a microneedle array, to increase potency. This array is a fingertip-sized patch of 400 tiny needles that deliver the spike protein pieces into the skin, where the immune reaction is strongest. The patch goes on like a Band-Aid and then the needles—which are made entirely of sugar and the protein pieces—dissolve into the skin.
“We developed this to build on the original scratch method used to deliver the smallpox vaccine to the skin, but as a high-tech version that is more efficient and reproducible patient to patient,” Falo said. “And it’s actually pretty painless—it feels kind of like Velcro.”
The system also is highly scalable. The protein pieces are manufactured by a “cell factory”—layers upon layers of cultured cells engineered to express the SARS-CoV-2 spike protein—that can be stacked further to multiply yield. Purifying the protein also can be done at industrial scale. Mass-producing the microneedle array involves spinning down the protein-sugar mixture into a mold using a centrifuge. Once manufactured, the vaccine can sit at room temperature until it’s needed, eliminating the need for refrigeration during transport or storage.
“For most vaccines, you don’t need to address scalability to begin with,” Gambotto said. “But when you try to develop a vaccine quickly against a pandemic that’s the first requirement.”
When tested in mice, PittCoVacc generated a surge of antibodies against SARS-CoV-2 within two weeks of the microneedle prick.
Those animals haven’t been tracked long term yet, but the researchers point out that mice who got their MERS-CoV vaccine produced a sufficient level of antibodies to neutralize the virus for at least a year, and so far the antibody levels of the SARS-CoV-2 vaccinated animals seem to be following the same trend.
Importantly, the SARS-CoV-2 microneedle vaccine maintains its potency even after being thoroughly sterilized with gamma radiation—a key step toward making a product that’s suitable for use in humans.
The authors are now in the process of applying for an investigational new drug approval from the FDA in anticipation of starting a Phase I human clinical trial in the next few months.
“Testing in patients would typically require at least a year and probably longer,” Falo said. “This particular situation is different from anything we’ve ever seen, so we don’t know how long the clinical development process will take. Recently announced revisions to the normal processes suggest we may be able to advance this faster.”



