All cancer cells—rather than just a subset—can enter a sluggish, slow-dividing state if they come under threat. Then, after the threat has passed, they can wake up and begin replicating at full tilt. By entering and leaving a dormant state in such coordinated fashion, the cancer cells can defeat a round of chemotherapy—and gain enough time to acquire resistance to additional rounds of chemotherapy.
Curiously, the cancer cells can act like an organism that is going through hibernation. But hibernation isn’t the right word. It’s diapause, a reversible state of suspended embryonic development triggered by unfavorable environmental conditions.
That cancer cells can, as a group, hijack diapause, a highly conserved developmental mechanism, was discovered by scientists affiliated with the Princess Margaret Cancer Center and the University of Toronto. These scientists, led by Catherine O’Brien, MD, PhD, and Miguel Ramalho-Santos, PhD, published their findings in an article (“Colorectal Cancer Cells Enter a Diapause-like DTP State to Survive Chemotherapy”) that appeared in the journal Cell.
“We combined cellular barcoding and mathematical modeling in patient-derived colorectal cancer models to identify and characterize drug-tolerant persister (DTP) states in response to chemotherapy,” the article’s authors wrote. “Barcode analysis revealed no loss of clonal complexity of tumors that entered the DTP state and recurred following treatment cessation.”
The scientists emphasized that their data fit a mathematical model where all cancer cells, and not a small subpopulation, possess an “equipotent capacity to become DTPs.”
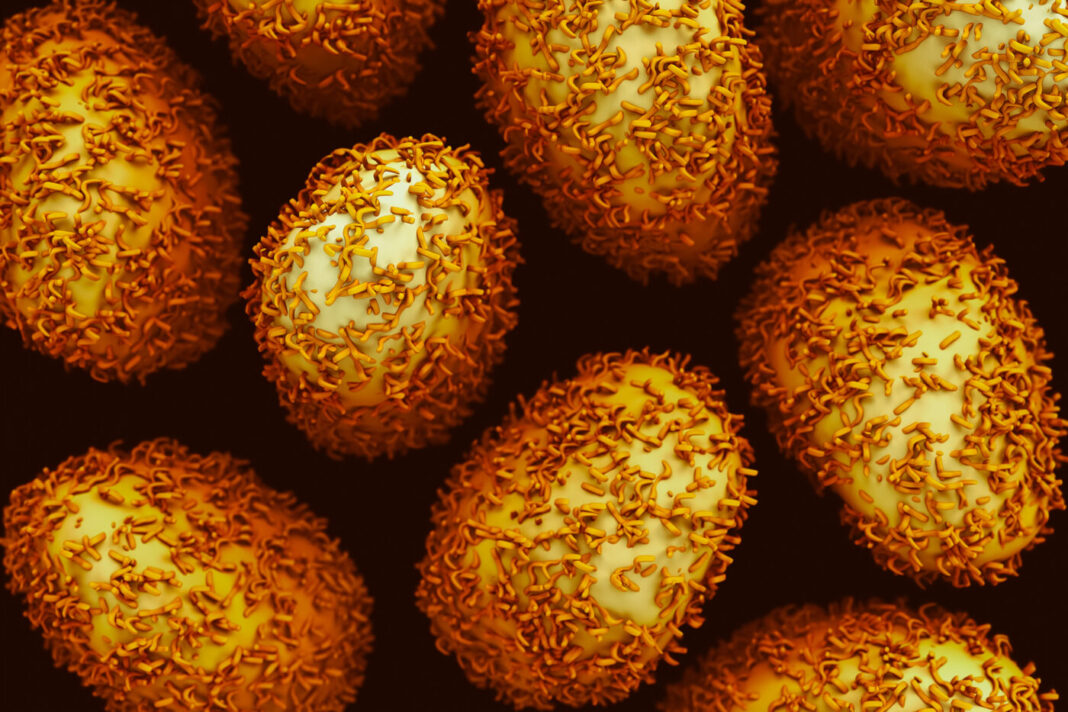
Human colorectal cancer cells in a petri dish were treated with chemotherapy. This induced a slow-dividing state across all the cancer cells in which they stopped expanding, requiring little nutrition to survive. As long as the chemotherapy remained in the dish, the cancer cells remained in this low-energy state, which the scientists described as a “diapause-like DTP state.”
It appears that the cancer cells can co-opt diapause, an embryonic survival program used by more than 100 species of mammals to keep their embryos safe inside their bodies in times of extreme environmental conditions, such as high or low temperatures or lack of food.
In this state, there is minimal cell division, greatly reduced metabolism, and embryo development is put on hold. Cancer cells in the DTP state, the scientists determined, “display remarkable transcriptional and functional similarities to diapause.”

Remembering a talk three years ago on cellular mechanisms driving this survival strategy in mouse embryos, O’Brien had an “Aha!” insight.
“Something clicked for me when I heard that talk,” she recalled. “Could the cancer cells be hijacking this survival mechanism to survive chemotherapy?”
So, O’Brien contacted the Toronto Mt. Sinai Hospital researcher Ramalho-Santos who had given the original talk at Princess Margaret. O’Brien compared the gene expression profile of the cancer cells in the chemotherapy-induced, slow-dividing state to the paused mouse embryos in Ramalho-Santos’ lab, and found that they were strikingly similar.
Similar to embryos, cancer cells in the slow-dividing state require activation of the cellular process called autophagy, meaning “self-devouring.” This is a process in which the cell “devours” or destroys its own proteins or other cellular components to survive in the absence of other nutrients.
O’Brien tested a small molecule that inhibits autophagy and found that the cancer cells did not survive. The chemotherapy killed the cancer cells without this protective mechanism.
“This gives us a unique therapeutic opportunity,” explained O’Brien. “We need to target cancer cells while they are in this slow-cycling, vulnerable state before they acquire the genetic mutations that drive drug-resistance.
“It is a new way to think about resistance to chemotherapy and how to overcome it.”