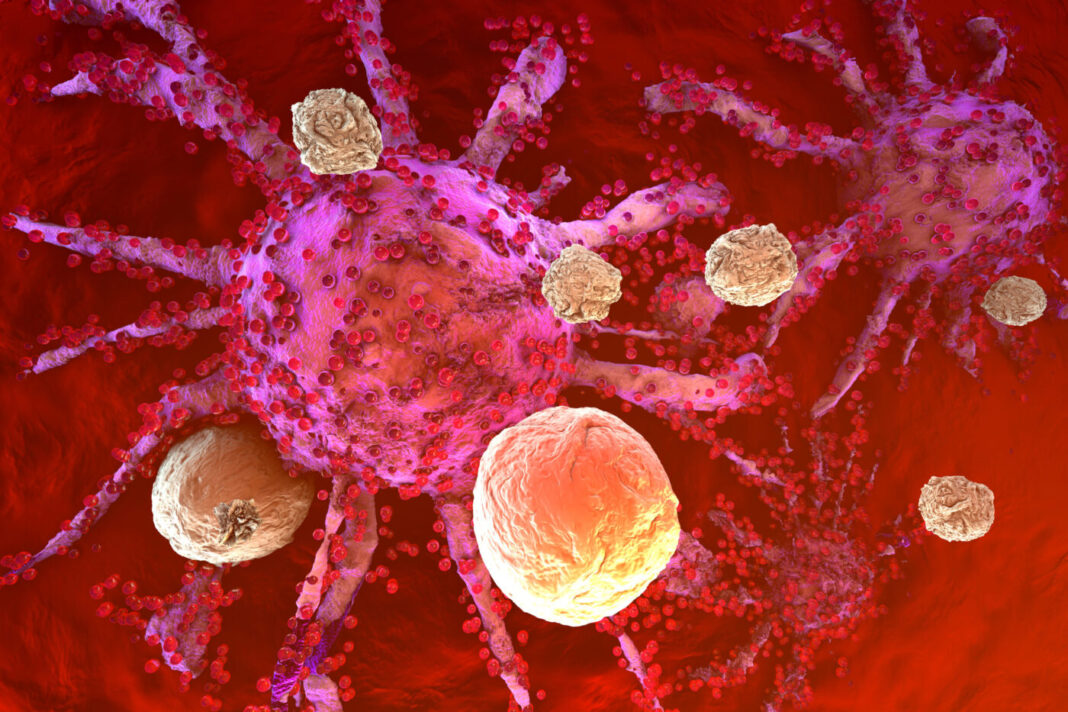
Immune exclusion, or the lack of immune cells in the vicinity of cancer cells, predicts poor patient outcomes in multiple cancers, including triple-negative breast cancer (TNBC). Now, researchers have identified a key molecule, discoidin domain receptor 1 (DDR1), that prevents immune cells from entering tumors and killing the cancer cells inside through the formation of the extracellular matrix (ECM). These findings could pave the way toward a new treatment for certain kinds of aggressive breast cancer.
This work is published in Nature, in the article, “Tumour DDR1 Promotes Collagen Fibre Alignment to Instigate Immune Exclusion.”
“During cancer progression, this molecule, known as DDR1, organizes a high-order extracellular matrix that acts like barbed wire around the boundary of a tumor to prevent immune cells from entering the tumor,” Rong Li, PhD, chair and professor in the department of biochemistry and molecular medicine at George Washington School of Medicine and Health Sciences. “Knowing that the DDR1 molecule creates a protective boundary around tumors, we were able to use preclinical models to show that the moment you deactivate DDR1, immune cells can infiltrate the tumor and kill the cells inside.”
Li and colleagues studied TNBC, an aggressive form of cancer that accounts for about 15% of all breast cancer cases. This type of cancer, according to the Centers for Disease Control and Prevention, lacks the receptors commonly used in targeted cancer therapies, making it difficult to target the tumor cells. Immunotherapy is designed to activate immune cells when they can get to the center of a tumor, but DDR1, a collagen receptor with tyrosine kinase activity, instigates immune exclusion by promoting collagen fiber alignment—putting up a physical barrier to anti-tumor immune cells. Identifying the underlying mechanism could provide a new way of looking for novel therapeutic agents for this hard-to-treat cancer, Li said.
The researchers assessed the impact of removing DDR1 in multiple preclinical models. They determined that knocking out DDR1 not only halts tumor growth, but it also may protect the body from future tumors. The authors wrote that ablation of DDR1 in tumors, “promotes the intratumoral penetration of T cells and obliterates tumor growth in mouse models of TNBC.” The authors noted that, in human TNBC, the expression of DDR1 negatively correlates with the intratumoral abundance of anti-tumor T cells.
The group also determined that the DDR1 extracellular domain, but not its intracellular kinase domain, is required for immune exclusion. Membrane-untethered DDR1 extracelluar domain is sufficient, they say, to rescue the growth of DDR1-knockout tumors in immunocompetent hosts.
In conjunction with the new findings, collaborator Zhiqiang An, PhD, director of the Texas Therapeutics Institute and professor at the University of Texas Health Science Center at Houston, has developed a therapeutic DDR1-targeting antibody that breaks down that line of defense and helps tumor-killing immune cells cross.
“The discovery of the important role of DDR1 in cancer resistance is a significant advance that can potentially transform treatment pathways,” said An. “I’m delighted by the collaboration between researchers and academic labs, excited by synergies of basic and translational research, and encouraged by the rapid translation from discovery to therapeutic candidates for the benefit of people living with cancer.”