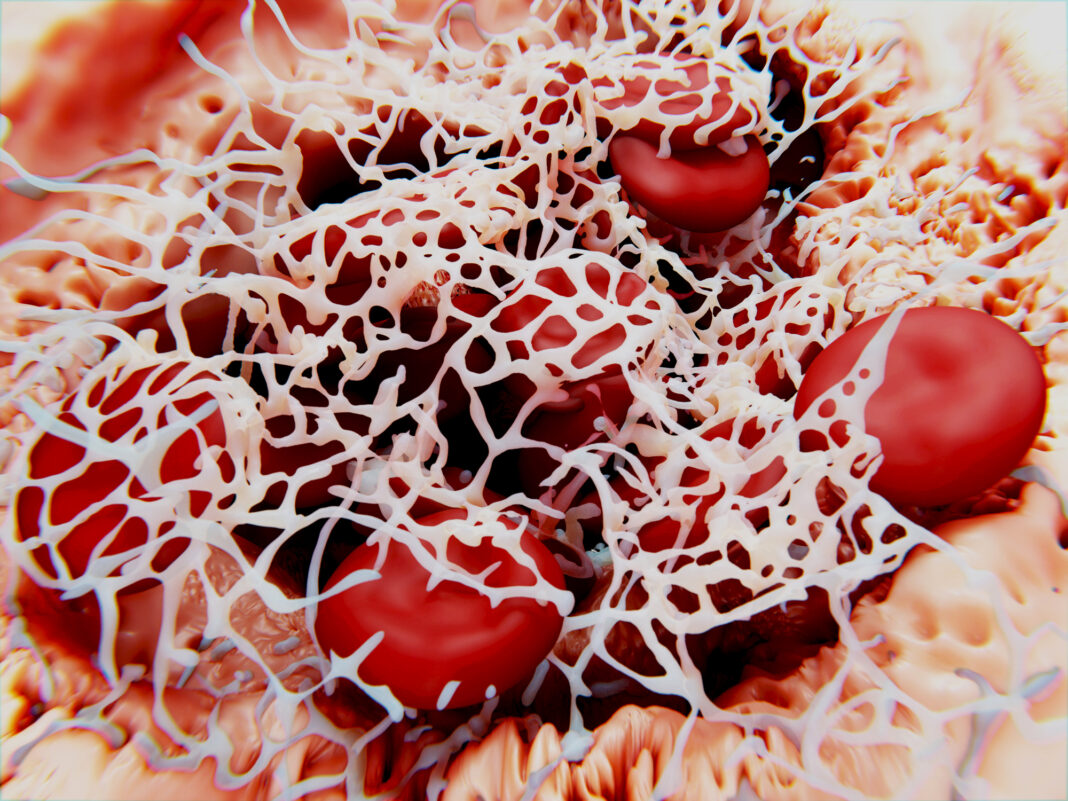
Fibrin plays a major role in stopping bleeding and healing wounds. However, if fibrin is formed in excess, e.g., in chronic wounds, thrombosis and subsequent vascular occlusions can occur. Therefore, the strict regulation of fibrin formation is important. How blood clots is limited and was not fully understood—until now.
University Hospital of Würzburg researchers and their collaborators say they have deciphered a central regulatory mechanism of fibrin formation and propose new therapeutic approaches. The results “Platelet glycoprotein V spatio-temporally controls fibrin formation” appear in Nature Cardiovascular Research.
“The activation of platelets and coagulation at vascular injury sites is crucial for hemostasis but can promote thrombosis and inflammation in vascular pathologies. Here, we delineate an unexpected spatio-temporal control mechanism of thrombin activity that is platelet orchestrated and locally limits excessive fibrin formation after initial hemostatic platelet deposition,” write the investigators.

“Genetic or pharmacologic defects in hemostatic platelet function are unexpectedly attenuated by specific blockade of GPV shedding, indicating that the spatio-temporal control of thrombin-dependent fibrin generation also represents a potential therapeutic target to improve hemostasis.”
GPV controls thrombin activity and fibrin formation
In this study, the research group led by Bernhard Nieswandt, PhD, identified a fundamentally new mechanism:
“For the first time, we were able to uncover a new switching point that regulates both hemostasis and thrombosis. This switch is glycoprotein V, GPV, which is expressed on the surface of blood platelets. GPV controls the activity of the enzyme thrombin, which is responsible for the formation of fibrin,” explains Nieswandt, head of the Institute of Experimental Biomedicine I and member of the board of the Rudolf Virchow Center, Center for Integrative and Translational Bioimaging (RVZ) at the University of Würzburg.
Thrombin is a crucial enzyme in blood clotting and its activity must therefore be precisely spatio-temporally controlled. Until now, it was known that the surface receptor GPV is cleaved by thrombin during platelet activation. This releases GPV as a soluble form.
However, the physiological function of this receptor was largely unknown. Using genetic and pharmacological approaches, the researchers showed that thrombin-mediated cleavage of GPV limits fibrin formation. By remaining bound to thrombin, soluble GPV alters the activity of thrombin so that it can form less fibrin.
In experimental thrombosis models, soluble GPV was shown to prevent, among other things, the formation of vaso-occlusive thrombi and to lead to a significant protection from experimental stroke and associated brain damage. Nieswandt is convinced that these new findings will change textbook knowledge.
Antibodies against GPV
The research group also generated antibodies against GPV that prevent thrombin-mediated cleavage of GPV.
“In our studies, we were able to show that these antibodies increase thrombin activity, resulting in increased fibrin formation. Our idea was therefore to use these antibodies in the context of impaired hemostasis to increase fibrin formation,” says David Stegner, PhD, head of the vascular imaging group at RVZ and one of the study’s last authors.
In addition to genetic causes, a reduced platelet count or impaired function can also be caused by pharmacological treatment and therefore lead to an impaired hemostasis. Treatment with platelet aggregation inhibitors, such as clopidogrel, which are used to prevent heart attacks or strokes and to treat circulatory disorders, e.g. impairs platelet function.
“In an experimental model of hemostasis, our new antibody was indeed able to restore hemostasis under conditions where hemostasis is otherwise not possible. This indicates a support of hemostasis by enhancing thrombin-dependent fibrin formation,” adds Sarah Beck, PhD, scientist at the Würzburg Institute for Experimental Biomedicine and first author of the study. “Anti-GPV treatment could have great clinical potential. This will be investigated in more detail in the future.”