San Diego State University (SDSU) researchers scraped tubeworms (Hydroides elegans) off the bottom of boats in the San Diego harbor and discovered that a beneficial bacterium that aids them in establishing colonies could also be a boon for human health because the same process might already take place in the human gut.
By examining this bacterium that causes metamorphosis in the tubeworm, marine microbiologists at SDSU found that the nanoscale syringe-like structures produced by it—a structure nicknamed the Death Star for the effect it has—could be used in the future to deliver novel therapeutics or vaccines to targeted cells and tissues in humans.
Nicholas Shikuma, PhD, assistant professor in the department of biology at SDSU, has been studying tubeworms for several years with students in his lab, to understand exactly why they are drawn to certain places in the ocean where they establish colonies. Previous research by others showed that like coral reefs, sea urchins, and sea squirts, the tubeworms also needed a conducive environment to reproduce, so they typically gravitated to areas with healthy populations of bacteria like Pseudoalteromonas, a beneficial bacterium.
Shikuma discovered that the bacterium has Metamorphosis Associated Contractile structures (MACs)—syringe-like structures that inject content into the larvae of tubeworms, helping transform it into juvenile worms.
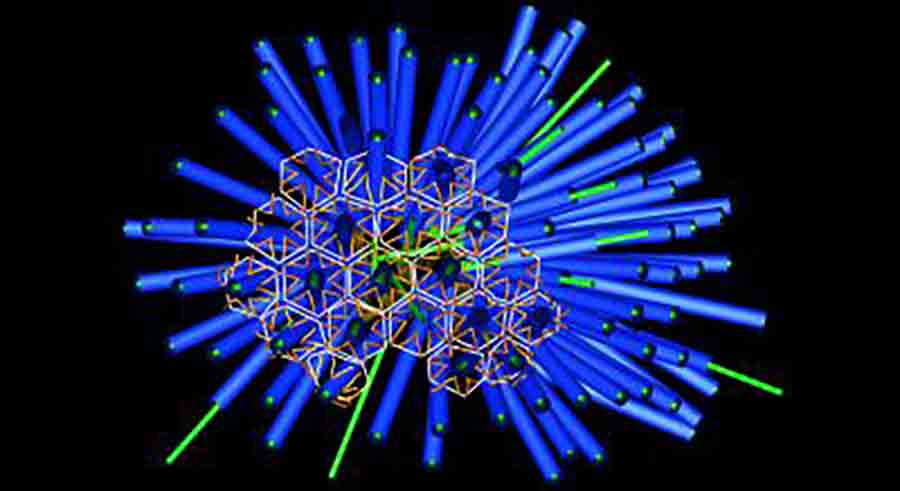
What he and fellow scientists did not know was if the MACs were injecting a biochemical into the tubeworm to cause metamorphosis and to stick to boat hulls. Shikuma’s lab used cryo-electron tomography imaging to study the structures and found arrays of death star shaped injection systems, which are released by the bacterium.
They found that the syringe structures contained a novel effector protein, Mif1, that regulates biological activity in the tubeworm host, and it’s this protein that’s responsible for causing metamorphosis.
The study (“A contractile injection system stimulates tubeworm metamorphosis by translocating a proteinaceous effector”) appears in eLife and follows on the heels of a recent publication from Shikuma’s lab that was published in Cell Reports in June which looked at how this bacterium interacts in vitro with insect and mouse cells. That paper showed how the microscopic syringe structures could be modified with payloads that could potentially carry therapeutics or vaccines.
“The swimming larvae of many marine animals identify a location on the sea floor to undergo metamorphosis based on the presence of specific bacteria. Although this microbe–animal interaction is critical for the life cycles of diverse marine animals, what types of biochemical cues from bacteria that induce metamorphosis has been a mystery,” the investigators wrote in the current paper.
“Metamorphosis of larvae of the tubeworm Hydroides elegans is induced by arrays of phage tail-like contractile injection systems, which are released by the bacterium Pseudoalteromonas luteoviolacea. Here we identify the novel effector protein Mif1. By cryo-electron tomography imaging and functional assays, we observe Mif1 as cargo inside the tube lumen of the contractile injection system and show that the mif1 gene is required for inducing metamorphosis. Purified Mif1 is sufficient for triggering metamorphosis when electroporated into tubeworm larvae. Our results indicate that the delivery of protein effectors by contractile injection systems may orchestrate microbe–animal interactions in diverse contexts.
“Lots of pathogens produce these syringe structures that typically cause disease,” Shikuma said. “But this is the first time we discovered bacteria that use the syringe for a symbiotic purpose.”
The MACs resemble similar syringe structures found on bacteriophages and with evolution, the bacteria have “stolen” this structure from the phages and have put it to good use.
“Phage typically attack bacteria with these structures, but instead of using it to infect other bacteria, the Pseudoalteromonas now uses it to interact with other animals, such as tubeworms, insects, and mouse cells,” explained Shikuma. “MACs are created when the bacteria undergo cell lysis and the bacteria that do this die afterwards, so it’s almost like altruism because it benefits the rest of the bacterial population.”
Not every bacterium in this strain produces the MACs, only about one out of 50 do so, but since we can produce trillions of these bacteria, supply will not be an issue and more of them can be engineered to produce MACs, he continued.
Shikuma has obtained a provisional patent for his findings on using the MACs to deliver modified proteins. As a next step, current research in his lab involves mining data from the Human Microbiome Project to see if we humans have this same bacterial syringe structure in our guts that can be harnessed for therapeutics.