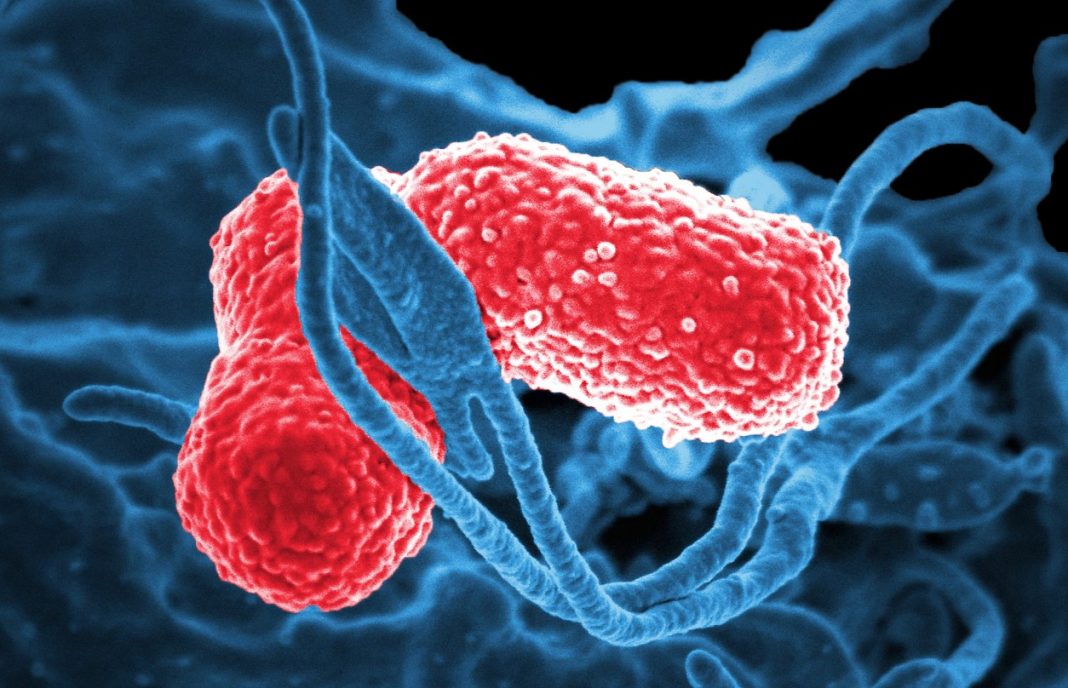
Researchers at Emory Health Sciences have detected “heteroresistance” to colistin, a last-resort antibiotic, in already highly resistant Klebsiella pneumoniae. Their study (“Carbapenem-Resistant Klebsiella pneumoniae Exhibiting Clinically Undetected Colistin Heteroresistance Leads to Treatment Failure in a Murine Model of Infection”) appears in mBio.
“Antibiotic resistance is a growing crisis and a grave threat to human health. It is projected that antibiotic-resistant infections will lead to 10 million annual deaths worldwide by the year 2050. Among the most significant threats are carbapenem-resistant Enterobacteriaceae (CRE), including carbapenem-resistant Klebsiella pneumoniae (CRKP), which lead to mortality rates as high as 40 to 50%. Few treatment options are available to treat CRKP, and the polymyxin antibiotic colistin is often the “last-line” therapy. However, resistance to colistin is increasing,” write the investigators.
“Here, we identify multidrug-resistant, carbapenemase-positive CRKP isolates that were classified as susceptible to colistin by clinical diagnostics yet harbored a minor subpopulation of phenotypically resistant cells. Within these isolates, the resistant subpopulation became predominant after growth in the presence of colistin but returned to baseline levels after subsequent culture in antibiotic-free media. This indicates that the resistance was phenotypic, rather than due to a genetic mutation, consistent with heteroresistance. Importantly, colistin therapy was unable to rescue mice infected with the heteroresistant strains.
“These findings demonstrate that colistin heteroresistance may cause in vivo treatment failure during K. pneumoniae infection, threatening the use of colistin as a last-line treatment for CRKP. Furthermore, these data sound the alarm for use of caution in interpreting colistin susceptibility test results, as isolates identified as susceptible may in fact resist antibiotic therapy and lead to unexplained treatment failures.”
David Weiss, Ph.D., director of the Emory Antibiotic Resistance Center, and his colleagues had observed heteroresistance to colistin in other bacteria, called Enterobacter, previously.
“This is concerning because Klebsiella is a more common cause of infection than Enterobacter, and these isolates were carbapenem-resistant, which means that they might actually be treated with colistin,” says Dr. Weiss, professor of medicine at Emory University School of Medicine and Emory Vaccine Center. “To our knowledge, this type of heteroresistant Klebsiella has not been observed in the United States before.”
The bacterial isolates came from urine samples from two patients in Atlanta-area hospitals as part of the nationwide Multi-site Gram-Negative Surveillance Initiative, part of the CDC-funded Emerging Infections Program.
Heteroresistance is caused by a minor subpopulation of resistant bacteria that are genetically identical to the rest of the susceptible bacteria, and it means that bacterial resistance to particular antibiotics is harder to monitor.
The bacterial isolates described in the mBio paper were not detectable with current diagnostic tests, although it was possible to see them by waiting an extra 24 hours for the resistant population to grow out. It appears that maintaining colistin resistance all the time is disadvantageous for bacteria. Probing the mechanism of heteroresistance, Dr. Weiss and his colleagues were able to see a signature of colistin resistance, in terms of genes turned on and off.
In a mouse model of peritonitis, infection with the heteroresistant isolates was lethal and untreatable by colistin. Colistin is viewed as a last resort measure for bacterial infections that are resistant to other drugs, partly because it is poisonous to the kidneys.
“Clinical laboratories should consider testing for heteroresistance to colistin if this last-line antibiotic is required for treatment,” the authors of the paper point out. However, they note that the extra time required is a downside. Novel diagnostics that rapidly and accurately detect colistin heteroresistance are needed.