Brain-wasting disorders often evoke a sense of fear and panic from both researchers and the general public alike. For scientists, this sense of dread stems from gaps in the knowledge base of the full pathogenesis for these diseases and a deficiency in effective treatments. What is understood, however, is the cause of wasting disorders like Creutzfeldt-Jakob disease (CJD)—the proteinaceous infectious particles called prions. Now, investigators at Case Western Reserve University School of Medicine (CWRU) have synthesized the first artificial human prion, a dramatic development in efforts to combat a devastating form of brain disease.
Findings from the new study were published recently in Nature Communications, in an article entitled “Artificial Strain of Human Prions Created In Vitro.”
“This accomplishment represents a watershed,” remarked senior study investigator Jiri Safar, M.D., professor of pathology and neurology at CWRU School of Medicine. “Until now our understanding of prions in the brain has been limited. Being able to generate synthetic human prions in a test tube as we have done will enable us to achieve a much richer understanding of prion structure and replication. This is crucial for developing inhibitors of their replication and propagation throughout the brain, which is essential for halting prion-based brain disease.”
Prions are proteins that have folded incorrectly. They can bind to neighboring normal proteins in the brain, triggering a domino effect that causes microscopic holes, turning brains into sponge and resulting in progressive deterioration, dementia, and certain death. There are numerous types of prion diseases in humans—CJD being the most common. Why and how human prion misfolding occurs has been a mystery that the Case Western Reserve investigative team may have solved with its new findings.
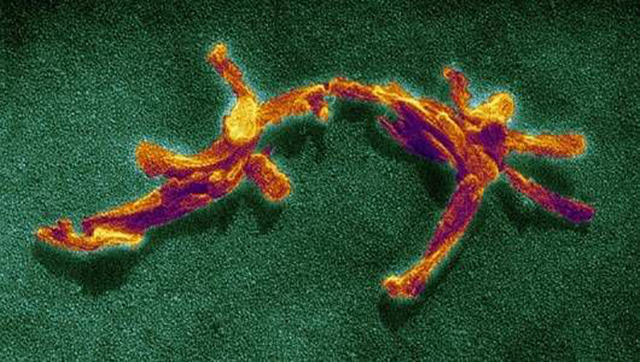
![Image of synthetic human prions accumulating in the brain of humanized transgenic mice. [Case Western Reserve School of Medicine]](https://genengnews.com/wp-content/uploads/2018/08/172357_web6665181342-1.jpg)
Image of synthetic human prions accumulating in the brain of humanized transgenic mice. [Case Western Reserve School of Medicine]
“We report the synthesis of new human prion from the recombinant human prion protein expressed in bacteria in reaction seeded with sCJD MM1 prions and cofactor, ganglioside GM1,” the authors wrote. These synthetic human prions were infectious to transgenic mice expressing non-glycosylated human prion protein, causing neurologic dysfunction after 459 and 224 days in the first and second passage, respectively. The neuropathology, replication potency, and biophysical profiling suggest that a novel, particularly neurotoxic human prion strain was created.”
Previous prion studies were carried out with laboratory nonhuman prions on mouse and hamster models. While this approach was useful for a general understanding of prion-triggered disease, human prions are different from these strains in both structure and mechanism of replication. Several recent therapeutic trials of human prion diseases have failed. Although these disappointing results may have occurred for multiple reasons, they demonstrate that the results from animal or cellular prion models do not automatically apply to human prions.
Creating artificial human prions will allow researchers to engage in an apples-to-apples study process, opening the door to more complete insights into how prions unleash their destructive force, potentially resulting in medications that can stop the disease in its tracks. And since Parkinson's and Alzheimer's diseases spread through the brain in a similar fashion as CJD, new inroads against these conditions are possible as well.
“Our findings explain at the structural level the emergence of new human prions and provide a basis for understanding how seemingly subtle differences in misfolded protein structure and modifications affect their transmissibility, cellular targeting, and thus manifestation in humans,” Dr. Safar concluded.