MacroGenics has acknowledged the deaths of seven patients in a Phase II trial it said it has halted assessing combinations of enoblituzumab (Fc-optimized B7-H3-directed monoclonal antibody) with either retifanlimab (anti-PD-1 monoclonal antibody) or tebotelimab (PD-1 × LAG-3 bispecific DART® molecule) as first-line treatments of patients with recurrent or metastatic squamous cell carcinoma of the head and neck (SCCHN).
The seven deaths “were potentially associated with hemorrhagic events in both arms of the study,” in which a total 62 patients were treated, MacroGenics said.
But of the seven deaths observed in the Phase II CP-MGA271-06 trial (NCT04634825), one event was assessed as possibly related to the study treatment—while the other six were evaluated as secondary to disease progression and/or unrelated to the treatment.
While fatal tumor-related hemorrhages and airway obstruction are known risks in patients with SCCHN, MacroGenics added that: “the incidence of fatal events observed in the study that were potentially hemorrhagic in origin was higher than what has been reported for this patient population in the medical literature.
That incidence is between 1% and 3.6%, according to a 2019 study—a range of incidence which, along with a risk-benefit analysis, led to the trial halt, MacroGenics added.
“Our top concern in conducting clinical trials is the safety of study participants,” said Scott Koenig, MD, PhD, president and CEO of MacroGenics. “We were surprised by the emergence of these events in first-line SCCHN patients, as we had not observed any such events in an earlier, smaller study in patients with later-line SCCHN disease who were treated with enoblituzumab in combination with an anti-PD-1 antibody.
MacroGenics said it was continuing to investigate and monitor these events, adding: “An analysis of the data is ongoing.”
MacroGenics has a co-development partner for enoblituzumab, Shanghai-based I-Mab, that holds rights to the drug for Greater China (China, Hong Kong, Macau and Taiwan).
Shares decline
Investors responded to the announcement of the clinical trials deaths by sending MacroGenics shares down nearly 11% in early trading Monday, to $3.12 a share as of 10:28 a.m., before rallying to send shares up to $3.55, a 1.4% gain from Friday.
The company added that it found no hemorrhagic events or coagulopathies seen in nonclinical toxicology studies of enoblituzumab, and the incidence of any fatal hemorrhage reported in earlier studies of enoblituzumab evaluated in over 340 patients across a broad range of tumor types was less than 1%.
Koenig said similar safety events had not been reported in patients treated with MGC018, the company’s B7-H3-targeted antibody-drug conjugate (ADC) molecule, licensed from Byondis.
As a result, the decision to close the CP-MGA271-06 study will not affect MacroGenics’ ongoing Phase 1/2 dose expansion study of MGC018 (NCT03729596) in patients with metastatic castrate-resistant prostate cancer (mCRPC), non-small cell lung cancer (NSCLC), squamous cell carcinoma of the head and neck (SCCHN) and melanoma. MacroGenics is also studying MGC018 plus lorigerlimab (an investigational PD-1 × CTLA-4 bispecific DART® molecule) in a Phase 1 study (NCT05293496) in patients with advanced solid tumors.
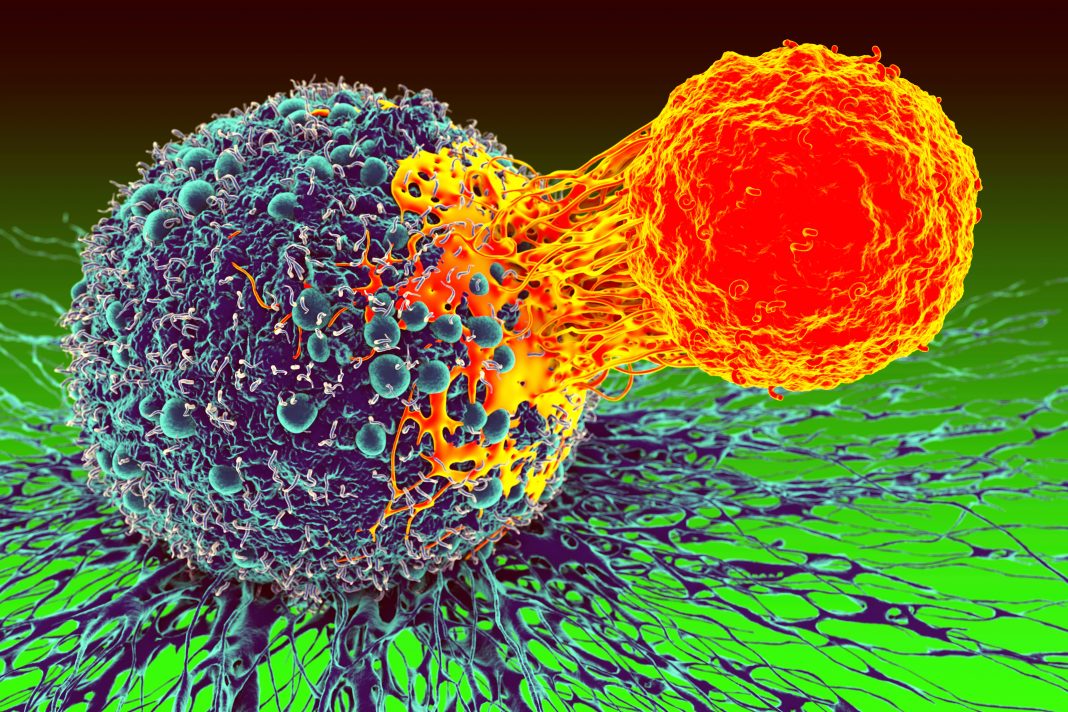
Enoblituzumab is an anti-B7-H3 monoclonal antibody that incorporates an immunoglobulin G1 fragment crystallizable (Fc) domain designed to enhance Fcγ receptor-mediated antibody-dependent cellular cytotoxicity. B7-H3, a protein in the B7 family of immune regulator proteins, is widely expressed by a number of different tumor types and, according to MacroGenics, may play a key role in regulating immune response to various types of cancer.
Retifanlimab is ananti-PD-1 monoclonal antibody being developed for use as monotherapy as well as in combination with other potential cancer therapeutics, which MacroGenics has licensed to Incyte Corporation in 2017 under a global collaboration and license agreement. Tebotelimab is a bispecific DART molecule designed to block PD-1 and lymphocyte-activation gene 3 (LAG-3) checkpoint molecules in order to sustain or restore the function of exhausted T cells.