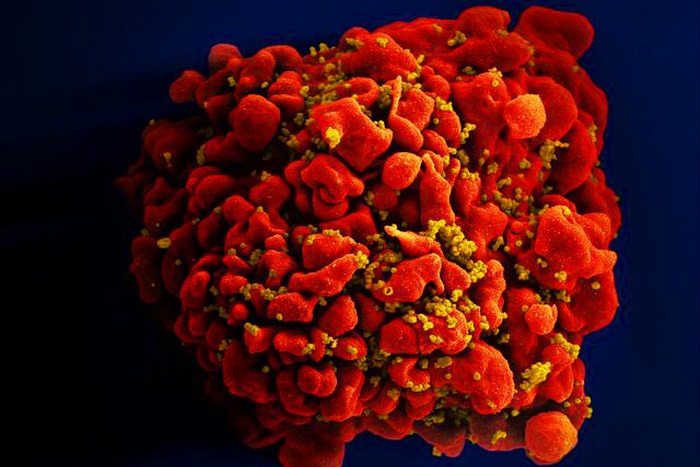
New research by scientists at the University of California, Los Angeles (UCLA), and colleagues suggests that new HIV infection may cut nearly five years off an individual’s lifespan compared to an uninfected person. The study shows how HIV has an impact on aging in infected people, accelerating biological changes in the body associated with normal aging within just two to three years of infection.
Their findings are published in the journal iScience in a paper titled, “Accelerated aging with HIV begins at the time of initial HIV infection.”
“Despite a significant increase in life expectancy, there is mounting evidence that living long-term with human immunodeficiency virus (HIV) and antiretroviral therapy, even when clinically well-controlled, is associated with an earlier than expected onset of chronic conditions such as heart and kidney disease, frailty, and neurocognitive difficulties,” wrote the scientists.
“Our work demonstrates that even in the early months and years of living with HIV, the virus has already set into motion an accelerated aging process at the DNA level,” said lead author Elizabeth Crabb Breen, a professor emerita at UCLA’s Cousins Center for Psychoneuroimmunology and of psychiatry and biobehavioral sciences at the David Geffen School of Medicine at UCLA. “This emphasizes the critical importance of early HIV diagnosis and an awareness of aging-related problems, as well as the value of preventing HIV infection in the first place.”
The scientists analyzed stored blood samples from 102 men collected six months or less before they became infected with HIV and again two to three years after infection. They compared these with matching samples from 102 non-infected men of the same age taken over the same time period. The authors say this study is the first to match infected and non-infected people in this way. All the men were participants in the Multicenter AIDS Cohort Study, an ongoing nationwide study initiated in 1984.
The scientists focused on how HIV affects epigenetic DNA methylation. The team examined five epigenetic measures of aging. Four of them are what are known as epigenetic “clocks.” The fifth measure assessed the length of telomeres.
HIV-infected individuals showed significant age acceleration in each of the four epigenetic clock measurements—ranging from 1.9 to 4.8 years—as well as telomere shortening over the period beginning just before infection and ending two to three years after, in the absence of highly active antiretroviral treatment. Similar age acceleration was not seen in the non-infected participants over the same time interval.
“Our access to rare, well-characterized samples allowed us to design this study in a way that leaves little doubt about the role of HIV in eliciting biological signatures of early aging,” said senior author Beth Jamieson, a professor in the division of hematology and oncology at the Geffen School. “Our long-term goal is to determine whether we can use any of these signatures to predict whether an individual is at increased risk for specific aging-related disease outcomes, thus exposing new targets for intervention therapeutics.”
The researchers noted some limitations to the study.
This study emphasizes the importance of recognizing how quickly the process of initial HIV infection begins accelerating epigenetic measures of aging, and lays a foundation for further exploration of characterizing these epigenetic measures as predictors of future clinical outcomes and impacts on health span.