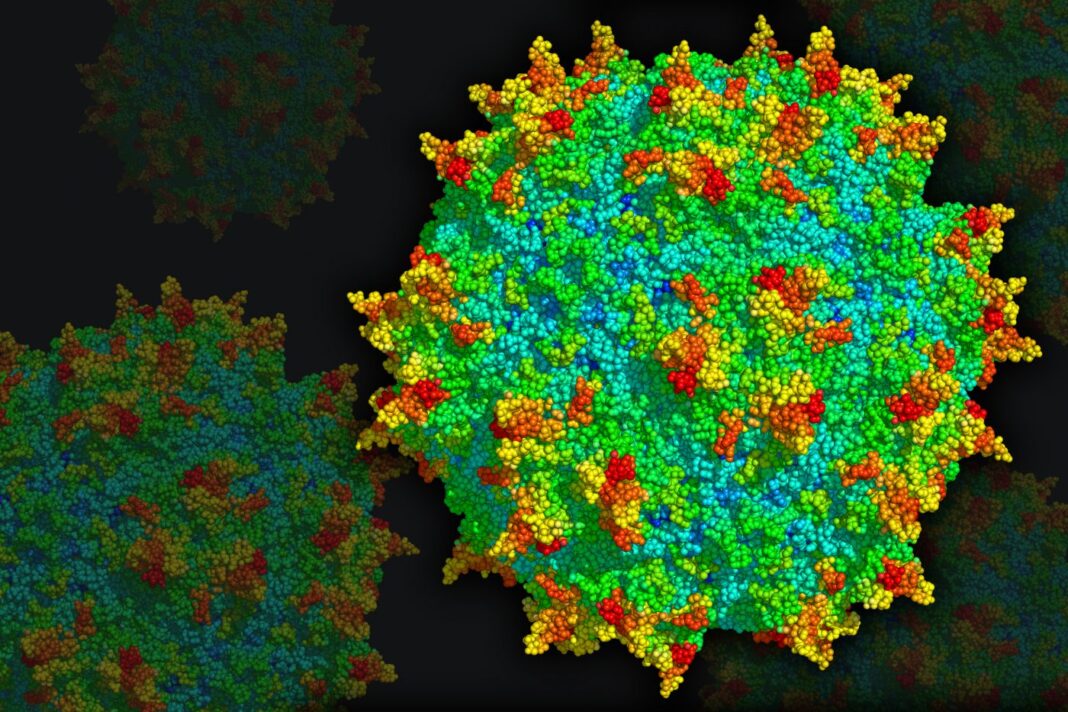
Although there are multiple viruses that can deliver genetic cargo to cells, adeno-associated viruses (AAVs) have become the workhorse of gene therapy delivery. Despite their promise in amplifying the current resurgence in gene therapy, and their role in two FDA-approved gene therapy products, AAVs are not without their limitations. Not only do they have a limited capacity for holding cargo, but, because AAVs are natural viruses, many people have antibodies to them which is problematic.
Now, a team of researchers has succeeded in inhibiting the immune response induced by AAV antibodies present as a result of natural immunity or following gene therapy. This result opens up new therapeutic prospects and the possibility of treating more patients.
The study, “IgG-cleaving endopeptidase enables in vivo gene therapy in the presence of anti-AAV neutralizing antibodies,” was published in Nature Medicine. The work was done by a team from Genethon, CNRS/Inserm, and Spark Therapeutics.
“This study represents an important step towards solving a complex and fundamental problem, namely the repeated administration of gene therapy treatments to patients who may need them, and also the treatment of patients who today are not eligible for gene therapy due to the existence of neutralizing antibodies in their systems,” says Frédéric Revah, PhD, CEO of Genethon.
In many cases, once it comes into contact with this virus, the body develops neutralizing antibodies. Between 30% and 50% of humans are naturally immunized against most AAVs used for therapeutic purposes. As a result, a large number of patients cannot currently benefit from AAV gene therapy. Moreover, a first injection of an AAV leads to an immune response against the vector, precluding any subsequent AAV gene therapy.
Strategies aimed at overcoming anti-AAV antibodies often involve immunosuppression and are not efficient in removing pre-existing antibodies. Imlifidase (IdeS) is an enzyme that is able to degrade circulating IgG. IdeS is currently being tested in transplant patients and the authors noted that they sought to determine if IdeS could eliminate anti-AAV antibodies in the context of gene therapy. The researchers used animal models to test the efficacy of IdeS.
The findings showed efficient cleavage of pooled human IgG in vitro upon enzyme treatment. The authors wrote that in mice passively immunized with intravenous Ig, “IdeS administration decreased anti-AAV antibodies and enabled efficient liver gene transfer.”
The approach was then scaled up to nonhuman primates, a natural host for wild-type AAV. Researchers injected the IdeS enzyme into subjects with neutralizing anti-AAV IgG before injecting the gene therapy vector of the same serotype and then observed that the IdeS treatment neutralized the action of the antibodies. This first step provided proof of the efficacy of this approach for subjects with natural immunity.
Then, the teams tested this approach with a view to the possible reinjection of gene therapy drugs. So, they administered a first dose of AAV vector, then a second dose after injection of IdeS. They observed that IdeS, by reducing the level of circulating antibodies, allowed the re-administration of the vector.
Finally, IdeS reduced anti-AAV antibody levels from human plasma samples in vitro, including plasma from prospective gene therapy trial participants.
The studies demonstrated that treatment with IdeS allows repeated administration of AAV gene therapy. This is a significant and promising step forward in the treatment of rare genetic diseases because, if the efficacy of this technique is confirmed in humans, it will make it possible to treat patients at the first signs of the disease and to re-inject a gene therapy product if necessary.
The results provide a potential solution to overcome pre-existing antibodies to AAV-based gene therapy.
“These studies should enable us to test this innovative approach in humans and thus, in the long term, to give AAV-positive patients the possibility of benefiting from gene therapy, despite the presence of antibodies,” noted Christian Leborgne, research engineer at Genethon. “This could also make it possible to treat patients as soon as the first symptoms of the disease appear (affecting the liver, for example) and, if necessary, to re-administer the gene therapy treatment in an effective manner.”