For millions of people living with diabetes, insulin is a life-saving drug, but it cannot be easily delivered as a pill; it needs to be injected under the skin using a syringe or pump. Researchers headed by a team at the School of Materials Science and Engineering, Sun Yat-sen University, and at the School of Pharmaceutical Sciences, Southern Medical University, Guangzhou, now report on the development of a new insulin micromotor (IMM) technology that allowed them to deliver insulin to the colons of rats using orally administered tablets powered by chemical “micromotors.”
Yingfeng Tu, PhD, Fei Peng, PhD, Kun Liu, PhD, and colleagues reported on tests with the motor-based mini-tablets in a paper in ACS Nano, in which they say the technology represents an “appealing strategy” that could feasibly be developed to improve the bioavailability of most biomacromolecular drugs. The paper is titled, “Micromotor Based Mini-Tablet for Oral Delivery of colleagues Insulin.”
Patients with diabetes have trouble regulating their blood glucose levels because they produce little or no insulin. Synthetic insulin has existed for over a hundred years, but it is often administered with an injection or an implanted pump. People affected by diabetes may need to take insulin multiple times per day, and frequent injections can be painful. As a result, some patients do not take the recommended dose at the correct times. “ …intensive insulin injection brings inadequate compliance, tissue infection, and increasing hypoglycemia risk that may induce brain damage, seizures, loss of consciousness, and even death,” the team wrote. “Hence, a convenient and effective insulin administration is urgently needed.”
An oral form of insulin would be ideal, but the harsh environment of the stomach breaks down and neutralizes the hormone before it can be absorbed by the intestines and get into the bloodstream. Absorption of large biomolecules through the gut lining is also hampered, the investigators added. “ … the existing intestine barrier composed of compact epithelial cells and a mucus layer further prevents the absorption of biomacromolecules due to their high molecular weight.”
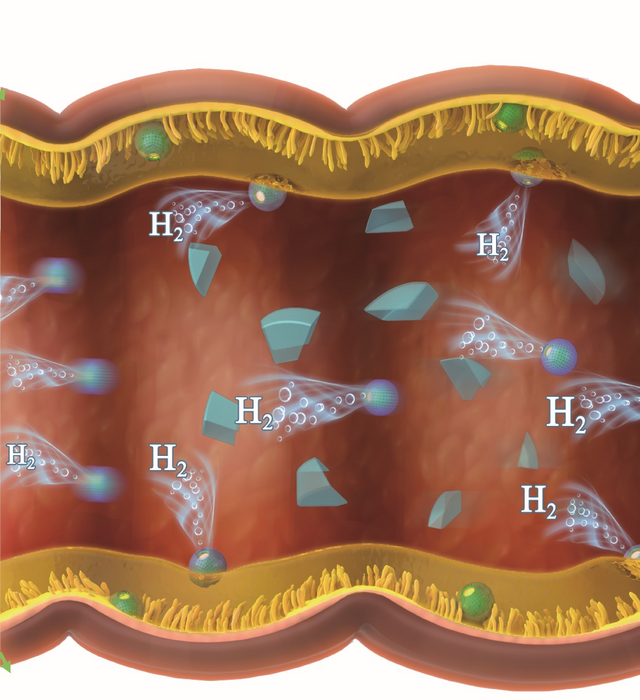
As part of the digestive system, the colon has a thinner mucosal layer and more loosely arranged epithelial cells, and displays milder digestive conditions. Previous attempts at oral administration, while protecting the hormone from stomach acids with micro- or nanocarriers, relied on insulin to passively diffuse into the cells that line the colon, which isn’t very efficient. “ … traditional micro/nanocarriers with passive diffusion result in limited insulin delivery efficiency,” the team acknowledged. In contrast, the newly developed insulin-loaded mini-tablets feature tiny, chemical “micromotors” that the preclinical tests showed could deliver insulin to the colon safely and effectively.
To make these tablets, the researchers covered magnesium (Mg) microparticles with a layer of an insulin-containing solution and a layer of liposomes. They then mixed these particles with baking soda, pressed them into mini-tablets that were about 3 mm long, then covered them with an esterified starch solution. The starch protects the tablets from stomach acid, allowing them to reach the colon intact. As they break down, the magnesium microparticles then react with water to generate a stream of hydrogen gas bubbles, which acts as micromotors that propel the insulin toward the colon’s lining to be absorbed. “Recently, Mg-based micromotors have been widely used due to the continuous production of hydrogen bubbles under local body fluids and subsequent generation of strong driving forces,” the authors noted. “By producing H2, the generated motion of the released IMMs resulted in enhanced colonic uptake and absorption of insulin, therefore resulting in higher oral bioavailability …
The team tested their mini-tablets in diabetic rats and found that they could significantly reduce the animals’ blood glucose levels for over five hours. “… the rapid locomotion of motors triggered by the local aqueous environment further resulted in enhanced mucosa penetration and active delivery of insulin, showing a stable blood glucose level for more than 5 h.” In fact, using the new insulin-delivery technology it was possible to maintain a glucose level almost as low as injection-delivered insulin.
Although more work is needed, the researchers say that their development represents a concrete step toward creating more oral formulations of traditionally injection-only medications. “The reduced dosing interval time and improved diabetes’ compliance of our system possibly make a concrete step toward the oral delivery of insulin for diabetes therapy,” they stated. “We believe that the proposed strategy with superior compliance, easy fabrication, an improved efficacy shows great potential for oral delivery of most biomacromolecular drugs … the easily tunable feature and biodegradability of Mg micromotors endow them fascinating applications in biomedical fields.”