June 15, 2017 (Vol. 37, No. 12)
Progenitor Cells Studies May Show the Path toward Curing Chronic Diseases
The promise of cell therapy for regenerative medicine is often viewed as being synonymous with stem cell therapy, but some companies are instead successfully bringing progenitor cell-based cell therapy approaches through preclinical and clinical development. They are targeting disorders that include type 1 diabetes, hearing loss, Duchenne muscular dystrophy (DMD), osteoarthritis, and multiple sclerosis, for example.
Innovative strategies that aim to deliver progenitor cells to patients may then rely on the cells’ ability to differentiate into healthy adult cells to restore missing tissue and function, or they may utilize the progenitor cells as vehicles for delivering growth factors and other signals to regenerate damaged tissue. Yet other novel approaches seek to identify small-molecule drugs that can stimulate the regenerative capabilities of progenitor cells that are already present in the body.
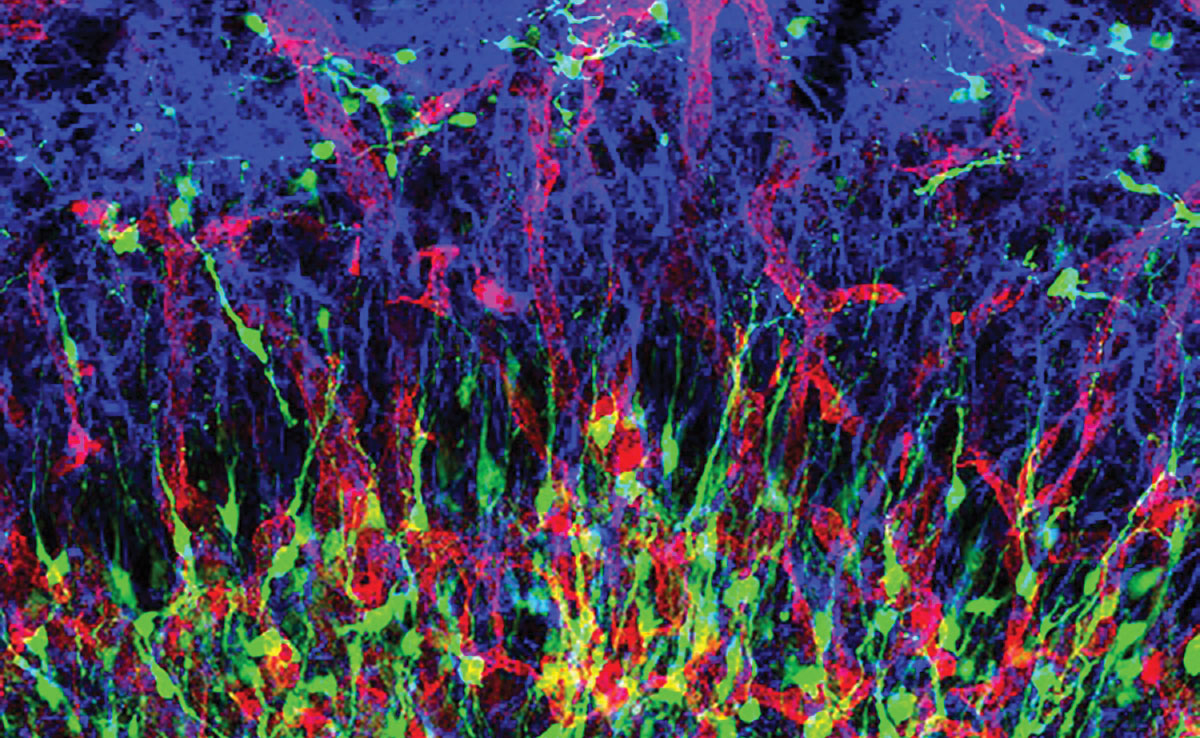
Confocal image of GFP-positive neural progenitor cells (green) in the rat olfactory bulb; RECA-1-positive blood vessels (red); and GFAP-positive astrocytes (blue). [Oleg Tsupykov / Wikimedia Commons]
Seeking a Cure for Diabetes
Type 1 diabetes (T1D) is the primary therapeutic focus of the stem cell-derived cell replacement therapies being refined by ViaCyte. The company has developed and standardized a manufacturing process that involves directed differentiation of embryonic stem cells to produce pancreatic progenitor cells, a product that it calls PEC-01™. When implanted subcutaneously, PEC-01 cells mature into pancreatic endocrine cells. They are able to form all five hormonal subtypes of pancreatic islet cells, including the insulin-producing beta cells and glucagon-producing alpha cells.
ViaCyte’s islet replacement therapy “has the potential to provide a functional cure for T1D as well as a treatment for patients with insulin-dependent type 2 diabetes,” says company President and CEO Paul Laikind, Ph.D. Unlike implanted cadaver-sourced islet cells, which have allowed some individuals with diabetes to live without the need for exogenous insulin for many years, “our approach provides an unlimited supply of cell material,” he adds.
ViaCyte is developing two PEC-01-based products. PEC-Encap™ fully encapsulates the progenitor cells in the retrievable Encaptra® cell delivery system that is designed to protect the cells from exposure to the patient’s immune system. With the PEC-Direct product, the cells are delivered in a device containing engineered pores that allow for direct vascularization and more robust engraftment. The cells in PEC-Direct are not protected from the immune system, and treated patients require immunosuppression.
PEC-Direct is targeted for use in patients with T1D who are at high risk for acute complications, such as hypoglycemia-unaware patients. ViaCyte will soon begin enrolling patients in the first phase I/II trial of PEC-Direct. “Over the next 12–18 months, we hope to show both proof-of-mechanism—that the cells are engrafting and differentiating as expected—and proof-of-efficacy, which will be insulin production, as measured by C peptide production and other endpoints such as reduced insulin utilization,” Dr. Laikind tells GEN.
Initial testing of PEC-Encap at subtherapeutic doses, in 19 patients in a STEP ONE trial, demonstrated the safety of the product and approach. “We put in ‘sentinels,’ small devices with small amounts of cells that we could withdraw periodically and do histology on to understand how the cells were faring in a patient,” says Kevin D’Amour, Ph.D., vice president of research and CSO of ViaCyte.
In addition to seeing no evidence of autoimmune or allogeneic rejection of the cells, the results showed vascularization, engraftment, and survival of the cells for at least three months, with differentiation into islet subtypes. Despite these encouraging findings, “engraftment was challenging and not consistent,” says Dr. D’Amour, and ViaCyte is working with materials science company W.L. Gore & Associates to improve the implantable device used to deliver PEC-01 cells and achieve better engraftment for PEC-Encap, which is targeted for use in all patients with T1D.
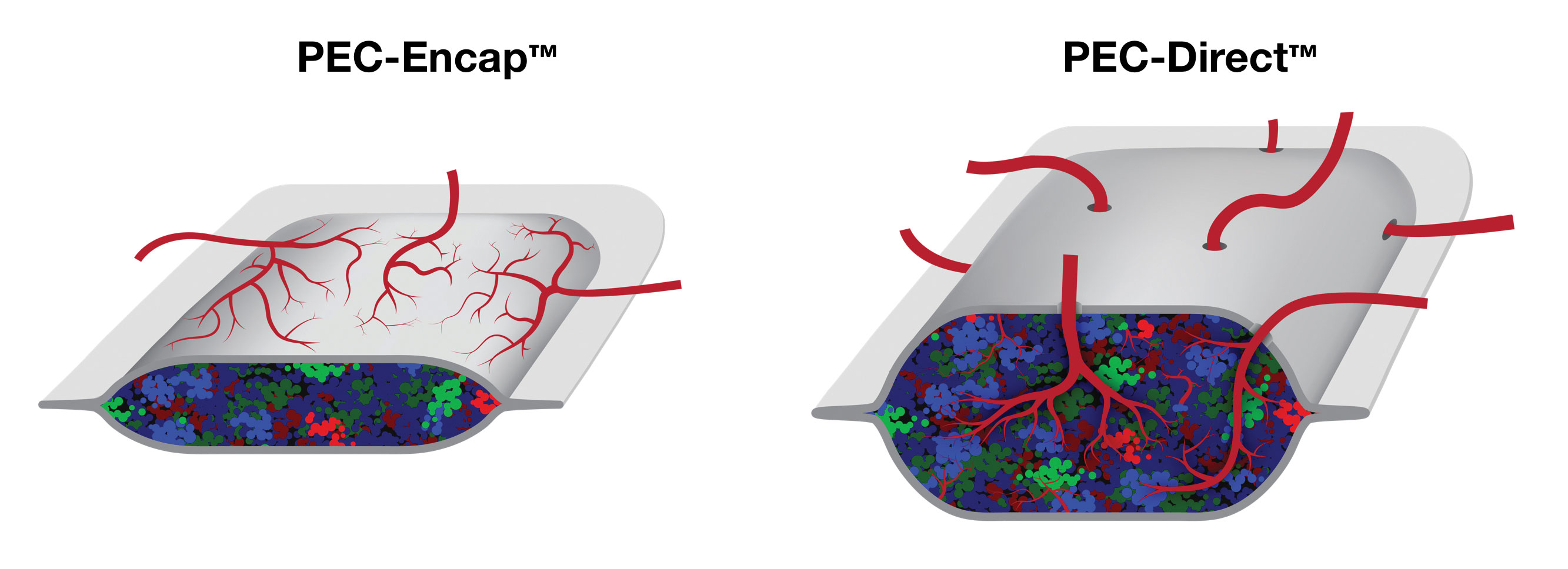
ViaCyte is developing a product called PEC-Encap™, or VC-01. It is designed to deliver pancreatic progenitor cells in an immunoprotective device. Another ViaCyte product candidate, PEC-Direct, delivers the pancreatic progenitor cells in a non-immunoprotective device that is designed for direct vascularization of the implanted cells.
Restoring Hearing
At Frequency Therapeutics, instead of starting with stem cells that have to differentiate or trying to deliver progenitor cells to a patient, the researchers are developing small-molecule therapeutics that can stimulate dormant progenitor cells already present “right where the body needs them,” says Chris Loose, Ph.D., co-founder and CSO of Frequency. The targeted progenitor cells, located in the inner ear in the case of Frequency’s lead regenerative medicine product, are “predestined to know how to make a certain kind of cell”—a functional hair cell with the capability to restore hearing in people with chronic hearing loss.
The work at Frequency builds upon the research of Robert Langer, Sc.D., and Jeff Karp, Ph.D., at MIT and Harvard Medical School on the Lgr5+ progenitor cell, first discovered in the epithelium of the gastrointestinal tract: a highly regenerative tissue, then shown to be present, but dormant, in the inner ear and the source of the cochlear hair cells essential for hearing.
Early on, the Frequency team considered the advantages of targeting the progenitors. One could stimulate them to become a little more stem-like and send them into their normal pathway [of asymmetric division], where they replace themselves and form the cell of interest . . . in this case, a hair cell. “Once you wake them up,” notes Dr. Loose, “they can follow much of the rest of the path on their own.” This thinking led to the progenitor cell activation (PCA™) platform, which Frequency describes as a controlled approach to activating “stemness” to stimulate Lgr5+ progenitor cells to divide and differentiate.
Unlike a genetic approach, which might turn these pathways on constitutively, using small molecules to achieve transient stimulation, so the progenitor cells divide, allows the effect to be “turned off” once the drugs are removed; but once formed, the hair cells could last a person’s lifetime. “There are no permanent genetic changes, which contribute to the safety of this approach,” Dr. Loose adds. Frequency delivers its drug via injection directly into the middle ear.
A recent article in Cell Reports (McLean et al. 2017;18[8]:1917–1929) demonstrates a + cells following small-molecule treatment and the formation of more than 11,500 hair cells from a single mouse cochlea, compared with less than 200 without treatment.
“We expect to be in the clinic within the next 12 months,” says David Lucchino, CEO. Frequency recently received $32 million in series A financing to support its clinical development program.
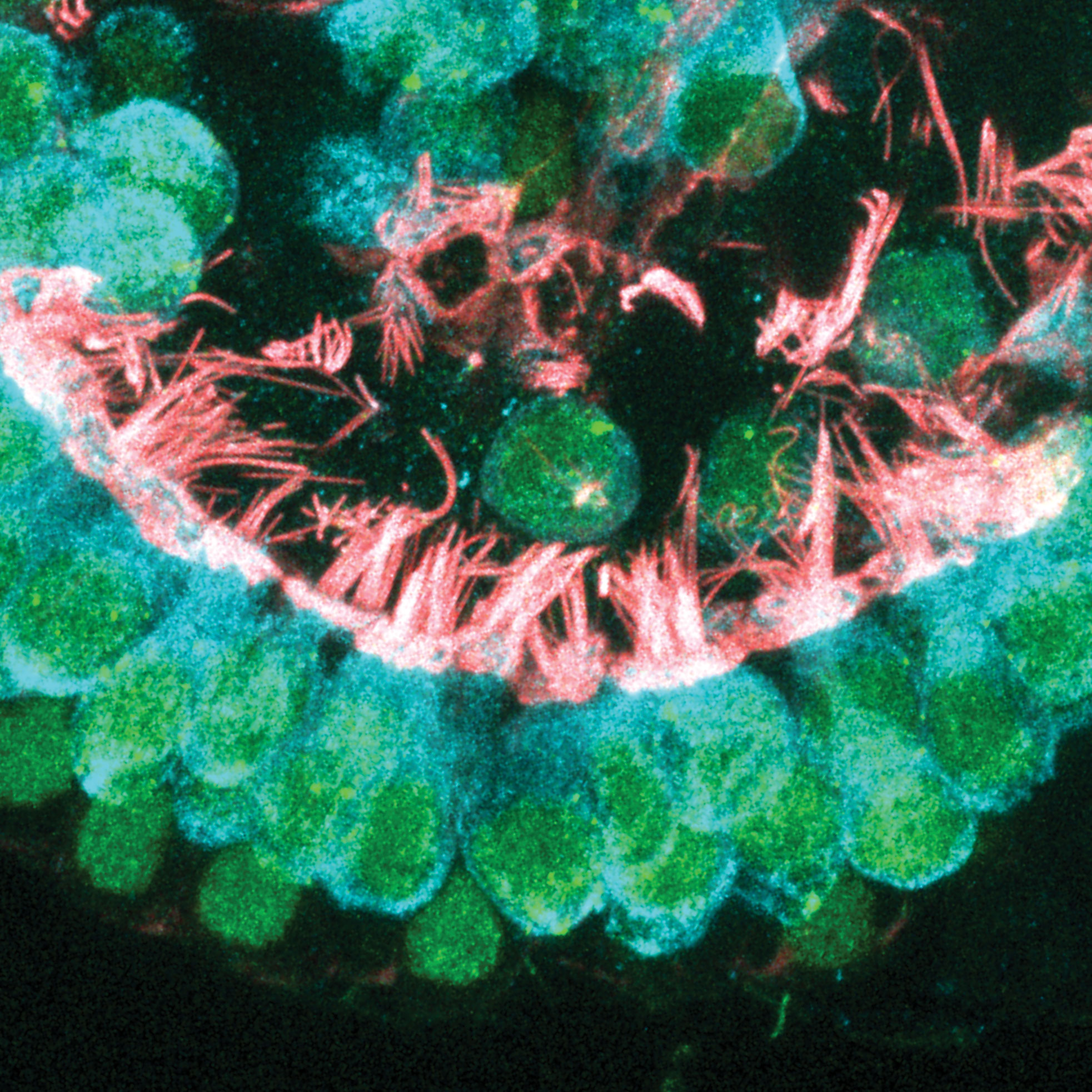
Frequency Therapeutics, a company that develops drugs to activate progenitor cells within the body and thereby restore healthy tissue, asserts that its work with academic partners has yielded a small-molecule approach to the regeneration of inner ear sensory hair cells. In this image, provided by Frequency’s Will J. McLean, Ph.D., newly formed cochlear hair cells contain intricate hair bundles with many stereocilia and other components that are critical for proper function and neural transmission.
Stimulating Progenitor Cells
Plasticell, a developer of cell therapies including hematopoietic cell-replacement therapies, recently announced a collaboration with Kings College London to initiate preclinical trials of its artificial blood platelet product, manufactured from pluripotent stem cells. Plasticell has also received funding from Innovate UK to support a £1.1-million project to manufacture red blood cells from pluripotent stem cells. The company uses its proprietary CombiCult® bead-based combinatorial screening technology to facilitate high-throughput differentiation of stem cells—human embryonic or induced pluripotent stem cells—into specific cell lineages.
Progenitor Therapeutics, a spinout of Plasticell, applies the CombiCult technology to generate progenitor cells,—which are usually present in very small numbers in the body,—which it then uses in its ProScreen™ drug-screening platform. In contrast to Plasticell’s cell-therapy approach to regenerative medicine, Progenitor’s goal is to identify small-molecule drugs that can stimulate progenitor cells to regenerate targeted tissues damaged by injury, disease, or aging. Progenitor is partnering with GlaxoSmithKline to screen GSK’s compound libraries. Initial therapeutic targets include osteoarthritis, multiple sclerosis, and muscular dystrophy.
“We have been identifying a lot of drug assets suitable for repurposing,” says Yen Choo, Ph.D., CEO of Plasticell and Progenitor Therapeutics.
Dr. Choo credits the GSK collaboration to the company’s proof-of-concept data in creating myeloid progenitors, the precursors to megakaryocytes and platelets, in sufficient quantity and purity to use in high-throughput drug screening to re-discover Promacta, GSK’s small-molecular regenerative drug that acts on the TPO receptor. The company has identified regenerative drug candidates for stimulating cartilage production that are ready to take into animal testing. The company’s program in multiple sclerosis targets oligodendrocyte progenitor cells in multiple sclerosis lesions to stimulate remyelination. Small molecules that can act on muscle progenitor cells are the focus of screening campaigns to identify drug candidates for muscle regeneration in DMD and post-surgical repair.
Exosomes for Muscle Regeneration
Capricor Therapeutics President and CEO Linda Marbán, Ph.D., describes the company’s regenerative medicine approach succinctly: “We take cardiospheres and turn them into cardiosphere-derived cells (CDC), a progenitor cell which can function as a local drug-delivery system.”
After the discovery of these cardiac-derived cells, the researchers found that they released growth factors, such as IGF-1, FGF, and VEGF, and when delivered systemically, these cells would travel to the site of tissue injury (i.e. to the heart in the case of myocardial infarction). While they persisted at the site of injury for a relatively short time, about a month, the benefits they delivered continued for many months. Capricor developed a method for producing allogeneic cardiosphere-derived cells from donor hearts and began testing the safety and efficacy of its CAP-1002 off-the-shelf product.
The “drugs” these cells are delivering are exosomes, says Dr. Marbán, “nanometer-size lipid bilayer vesicles packed with RNAs and some proteins that epigenetically modify cellular proteins such that they can change the behavior of a cell.” Capricor is developing the exosomes as a separate, second product pipeline.
When released by the CDCs, the exosomes are quickly taken up by neighboring cells. The results suggest that the exosomes are “epigenetically modifying protein expression, not changing the genes themselves, and in that way changing the behavior of the cells that are endogenous to the space,” Dr. Marbán says. “We also think the cells themselves put out an alarm bell for natural stem cells to arrive on the scene and repair tissue.”
Early clinical results with CAP-1002 from the CADUCEUS trial in patients who experienced a massive heart attack showed a significant reduction in scar size and significant increases in muscle mass at the affected area, which lasted at least a year after a single administration of CAP-1002. However, a recent interim analysis of data from the Phase II ALLSTAR trial in adults who experienced a massive heart attack showed that treatment with CAP-1002 was unlikely to achieve the primary efficacy endpoint of change in infarct size.
These results have led Capricor to focus its resources on its other ongoing clinical development program for CAP-1002, as a treatment for patients with DMD. The company recently released six-month results from the 25-patient randomized Phase I/II HOPE trial in young males with DMD with advanced cardiac disease. The results showed significant improvement in some measures of cardiac and upper-limb function compared to usual care. Capricor hopes to initiate a repeat-dose clinical trial of intravenous CAP-1002 in DMD in the second half of 2017 that would primarily evaluate the effects of treatment on skeletal (noncardiac) muscle function.
Regenerating the Body with Drugs
Essential parts of the human body’s regeneration machinery are adult stem cells (or progenitor cells) that reside in our tissues and are capable of differentiating into replacement cells that maintain organ function following disease or injury. The molecular pathways that cause tissue repair or regeneration can be complex and few are well understood.
However, there are well-known examples of simple biochemical stimuli that regenerate specific tissues. Perhaps the best is erythropoietin (EPO), a growth factor produced by oxygen-sensitive cells in the kidney, which stimulates hematopoietic erythroid progenitor cells to differentiate into red blood cells. A related growth factor, thrombopoietin (TPO), signals myeloid progenitor cells to differentiate into platelets that produce platelets, essential for blood clotting. Both EPO and TPO are natural growth factors that can be used clinically to regenerate specific cell types.
While EPO became the first blockbuster recombinant biologic drug, TPO was superseded in development by a synthetic chemical mimetic (Promacta®, GSK) that is orally available and less immunogenic. Promacta showed that a small-molecule drug can be used to
regenerate tissues of the body. What is the prospect, therefore, to develop such drugs further?
“High-content screening of human progenitor cells can be used to discover compounds that stimulate differentiation to specific cell types required to regenerate ailing organs,” says Yen Choo, Ph.D., founder and executive chairman of Plasticell and founder and CEO of Progenitor Therapeutics. While cell-based screening has multiple advantages in drug discovery, many of the progenitor cells of interest are relatively rare, or difficult to isolate, or both.”
According to Dr. Choo, companies like Progenitor generate rare progenitor cells for screening using more abundant pluripotent cells (e.g., human embryonic stem cells (hESC) or induced pluripotent stem cells (iPSC) as starting material. “
“This strategy has been used to create and screen high quality human progenitors from cartilage, myelin, and muscle—and regenerative drugs have been discovered to treat indications such as osteoarthritis, multiple sclerosis and muscular dystrophies,” added Dr. Choo.
Cancer Drug Holds Promise for Treating Allergies
Researchers at the Northwestern University Feinberg School of Medicine have found that a drug typically used to treat certain types of leukemia and lymphoma can also prevent reactions to some of the most common allergic reactions. Findings from the new study—published recently in the Journal of Allergy and Clinical Immunology in an article entitled “Ibrutinib, a Bruton’s Tyrosine Kinase Inhibitor Used for Treatment of Lymphoproliferative Disorders, Eliminates Both Aeroallergen Skin Test and Basophil Activation Test Reactivity”—could also have even greater implications for adults with food allergies.
The scientists discovered that cancer patients who were allergic to allergens such as cat dander and ragweed saw their allergic skin test reactivity reduced by 80% to 90% in 1 week, and this persisted with continued use of the drug for at least 1 to 2 months.
“It almost completely knocked out the patients’ skin test and blood cell allergic reactivity,” remarked senior study investigator Bruce Bochner, M.D., professor of medicine at Northwestern University Feinberg School of Medicine.
In the current study, Dr. Bochner and his colleagues performed traditional allergy skin tests and the basophil activation test, a related allergy test using blood cells, on cancer patients before they had taken the drug ibrutinib, 1 week after use, and again after 1 to 2 months of continued use. Ibrutinib is an FDA-approved drug currently approved as a successful and less toxic alternative to chemotherapy for patients with chronic lymphocytic leukemia and mantle cell lymphoma.
Previous research on ibrutinib told the researchers that the compound was a generally well-tolerated cancer drug successful in blocking a protein within cells called Bruton’s tyrosine kinase (BTK). BTK plays a crucial role in B-cell activation, growth, and maturation and mast cell and basophil activation, the latter two cells being responsible for immediate allergic reactions. The investigators focused on whether this BTK inhibitor could also shut down an enzyme inside cells that is involved when you have an allergic reaction.



