Targeted protein degradation is an emerging technology that has the potential to treat cancer and other diseases in a novel way. Like traditional inhibiting drugs, protein degraders are small molecules. However, they differ from other existing modalities in the way that they harness the cell’s natural recycling systems to degrade disease-causing proteins.
A succinct description of this new therapeutic approach is offered by Chris Nasveschuk, PhD, senior vice president of chemistry at C4 Therapeutics. He says, “You target those proteins that are causing disease and wipe them out.”
Most targeted protein degraders make use of what is called the ubiquitin-proteasome system, which can be thought of as the recycling system of the cell. However, as will be discussed here, a second protein-degrading pathway is now being explored that involves endocytosis, the process by which substances are brought into the cell.
A wide variety of questions about targeted protein degraders is now arising. To begin with, it is not clear what advantage this modality may have over traditional inhibitors that are already on the market. Furthermore, it is uncertain how this emerging class of drugs will perform in upcoming clinical trials. Will they prove to be safe and effective? To get a better understanding of these issues, GEN interviewed experts from five companies to get their views about this exciting new field.
The two flavors of targeted protein degradation
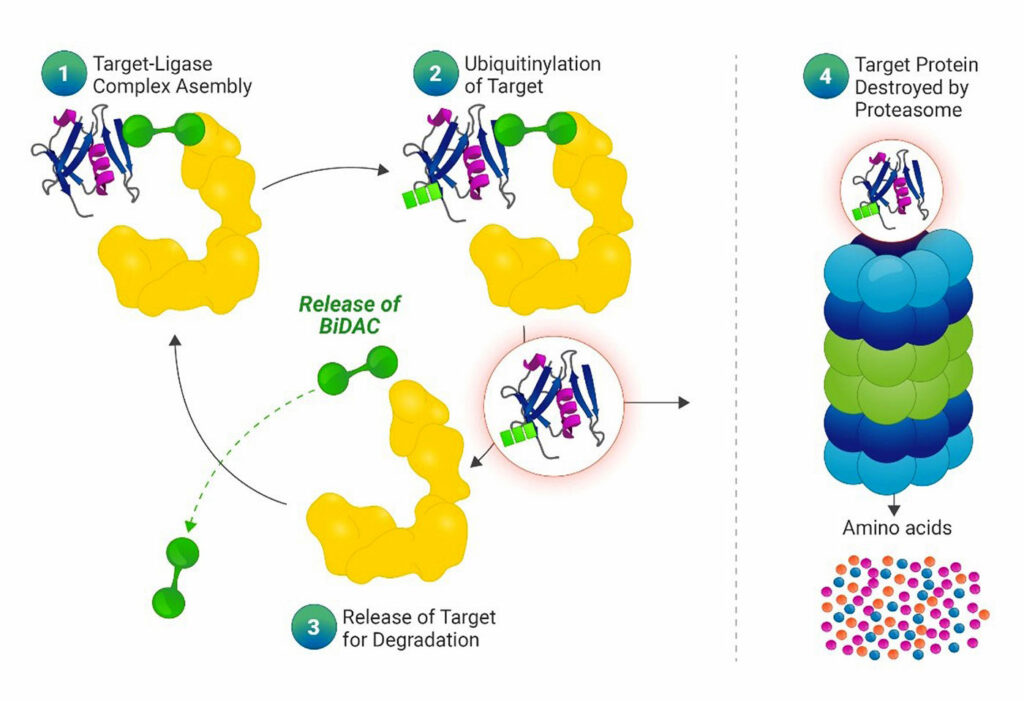
Most of the companies we interviewed were developing two main types of targeted protein degraders: proteolysis-targeting chimeras (PROTACs) and molecular glues. Both classes make use of the ubiquitin-proteasome system. The purpose of this system is to eliminate misfolded, damaged, and overabundant proteins with a cascade of distinct steps that ultimately involves an enzyme called the E3 ubiquitin ligase. This enzyme promotes the transfer of ubiquitin onto a lysine of the substrate protein. Multiple ubiquitination events signal the death knell for the faulty protein, which is then degraded by the proteasome, the so-called trash can of the cell.
PROTACs were first developed about 20 years ago. These molecules are referred to as being heterobifunctional because they consist of two different ligands. One ligand is designed to bind to the protein of interest, whereas the other binds to the E3 ubiquitin ligase. This binding then results in the protein being ubiquitinated and proteasomally degraded.
Although molecular glues are not heterobifunctional like PROTAC molecules, they work based on the same underlying mechanism: the ubiquitination of a protein of interest with the help of an E3 ligase. The most well-known molecular glue is thalidomide, which has received extensive negative publicity due to its tendency to cause birth defects. Nevertheless, thalidomide and its analogs are still used to treat multiple myeloma, and many companies continue to develop molecular glues for different diseases.
Why use a protein degrader?
Targeted protein degraders appear to have distinct advantages over more traditional inhibiting drugs. “Compared to traditional inhibitors, degraders have some potential advantages, such as eliminating scaffolding function, improving potency, and enhancing selectivity,” explains Yu Shen, PhD, director of cancer biology at AbbVie.
Another major advantage of protein inhibitors is that they have the potential to treat what are referred to as undruggable proteins. As Nasveschuk points out, “There are some proteins that are just not targetable through ligands. These are ideal targets for protein degradation.”
In some cases, the protein’s active site has a geometry that is not readily accessible. In other instances, although it may be possible to bind to a portion of a protein, there is no functional consequence of that binding event. “So, your inhibitor or ligand doesn’t actually do anything to the protein or modulate the disease,” Nasveschuk remarks. Protein degraders represent a novel way to target these undruggable proteins.
Experimenting with E3 ligases
Cereblon is an E3 ligase that is recruited by many targeted protein degraders, including thalidomide. “Cereblon’s advantages include the fact that it is widely expressed within blood cell types, making it ideal for engaging when treating hematologic malignancies,” says Gwenn M. Hansen, PhD, chief scientific officer at Nurix Therapeutics. She adds that Nurix has designed two protein degraders that both harness cereblon.
Over 600 E3 ligases are encoded in the human genome, and some of them may turn out to valuable in therapeutic applications. To explore this possibility, Nurix is testing a wide variety of E3 ligases in the construction of novel degraders. As Hansen notes, “In the future, we hope to develop degraders that harness unique E3 ligases with different properties that make them better suited for specific therapeutic indications.”
Incorporating antibodies
Shen notes that PROTACs have the potential to treat virtually any disease. However, due to permeability issues, they may be more feasible for some diseases than others. For instance, compared with small-molecule inhibitors, it may be challenging to develop oral PROTACs with good brain penetration.
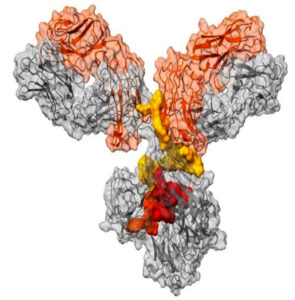
James Palacino, PhD, head of oncology at Orum Therapeutics, observes that “one challenge with a small-molecule protein degrader is that both the tumor and healthy tissue are exposed, leading to degradation of the target protein in a non-tissue-specific manner.” To improve the precision of delivery, Orum Therapeutics has developed a new therapy that involves a targeted protein degrader conjugated to an antibody.
Palacino believes that Orum’s approach for the targeted delivery of heterobifunctional degraders—referred to as Dual-Precision Targeted Protein Degradation (TPD2)—can overcome the solubility and permeability challenges associated with these molecules. He notes that “preclinical studies have demonstrated that Orum’s TPD² approach can deliver a potent and selective GSPT1 degrader molecule with improved pharmacokinetic and safety profiles.” This is important, he explains, because the loss of GSPT1 (by CRISPR knockout) has been shown to be broadly toxic to a panel of cancer cell lines.
A protein degrader with a very different mechanism
The protein degraders discussed thus far target the ubiquitin-proteasome system to eliminate damaged proteins. However, Avilar Therapeutics is developing a class of protein degraders known as asialoglycoprotein receptor (ASGPR)-targeting chimeras (ATACs) that work based on a very different mechanism. As Effie Tozzo, PhD, Avilar’s chief scientific officer, explains, “ATACs leverage a different natural system in the body—the endolysosome—for targeted protein degradation.” The endolysosome is the product of the fusion of an endosome and a lysosome during endocytosis.

Like PROTACs, ATACs are heterobifunctional drugs. One part of the ATAC binds to the protein targeted for degradation, whereas the other part binds to a receptor—as opposed to an E3 ligase—on the surface of hepatocytes. Tozzo explains that ASGPR is a scavenger receptor found on the surface of hepatocytes that mediates the process of endocytosis. Ultimately, Avilar’s approach with ATACs may treat hepatocellular carcinoma, the most common type of liver cancer.
What about safety and efficacy?
Twenty years have passed since the first PROTAC was reported, and many companies have brought protein degraders to preclinical and clinical development. This leads to the crucial question of whether new generations of targeted protein degraders are safe and effective.
Shen points out that no major safety-related issues have been observed with PROTAC drugs in clinical programs. He does not anticipate any major safety issues with ATAC degraders, even though clinical data on PROTAC safety is still limited, especially with respect to long-term outcomes. Shen’s optimism is shared by Tozzo. “By leveraging ASGPR,” Tozzo says, “we are engaging the natural machinery that the body is already using for protein degradation.”
Another key question involves whether the efficacy of various protein degraders may diminish over time. In the case of PROTACs, Shen notes that there is no evidence from clinical trials that they are more prone to resistance development than standard inhibitors. However, preclinical studies suggest that defects in the E3-ubiquitination system could become a source of resistance to PROTACs. As Shen explains, “Time will tell whether any of the resistance mechanisms observed in preclinical studies may emerge in the clinical setting.”
Despite the many unknowns, the companies we interviewed were optimistic about the prospect of clinical trials for their targeted protein degraders. Nasveschuk notes that C4 Therapeutics has three projects that are in Phase I trials, and multiple other drugs in the preclinical stage. Hansen also emphasizes the success of Nurix’s therapies that degrade a protein called Bruton’s tyrosine kinase (BTK). She notes that the company’s lead BTK degrader, NX-2127, has already demonstrated proof of efficacy in ongoing Phase I trials: “Thus far, we have demonstrated rapid, robust, and sustained BTK degradation independent of BTK mutations.”
Tozzo likewise suspects that ATAC inhibitors will perform well in clinical trials. She states, “Based on the robust degradation we have observed in our nonhuman primate studies with our proof-of-concept ATAC degraders, we anticipate good translation of ATAC
degradation activity in the clinic.”
The future of targeted protein degradation
There are compelling reasons to believe that targeted protein degradation—involving both the ubiquitin-proteasome system and the endolysosome system—will prove to be efficacious and safe for the treatment of various cancers. Nasveschuk concludes that this new therapeutic modality is going to be here for the “long haul,” even though he is unsure whether the molecules currently in clinical trials will reach the market. He declares, “This is a very exciting time for the field.”