Effective treatments for incontinence are urgently needed. Now, a multi-institutional team of researchers has developed a wireless system that can measure bladder function in freely moving rats over days to weeks. It can then use that real-time information to identify pathological voiding behavior and deliver a corrective signal in real time, in a closed-loop fashion. The implantable device provides a “set it and forget it” neuromodulation that delivers intermittent therapy that can diminish the urge to urinate, only when it is needed, and without any outside intervention.
The researchers from the Washington University School of Medicine in St. Louis, the University of Illinois at Urbana-Champaign, and the Feinberg School of Medicine at Northwestern University in Chicago, developed an approach that uses techniques in optogenetics, soft electronics, data analytics, and wireless powering/communication technologies to address overactive bladder in animals. This technology could be used for people who suffer from bladder problems and could even extend beyond the bladder to other tissues and organs of the body.
The work was published in a paper titled, “A wireless closed-loop system for optogenetic peripheral neuromodulation” in Nature on January 2.
The device is a strain gauge (a soft, stretchy belt-like device) that is implanted so that it wraps around the bladder (nothing is actually implanted into the bladder.) It is engineered so that the electrical resistance increases as it stretches and decreases as it relaxes. In turn, the strain gauge measures size changes of the bladder, not pressure inside the bladder. However, the bladder pressure correlates directly to the resistance measured with the strain gauge. So, when the bladder is filling and pressure in the bladder is increasing, the strain gauge signals this with an increase in resistance, and when the bladder empties and thus bladder pressure is decreasing, the bladder gets smaller, and the strain gauge signals this by a decrease in resistance.
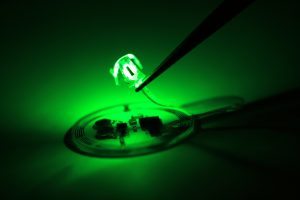
“When the bladder is emptying too often, the external device sends a signal that activates micro-LEDs on the bladder band device, and the lights then shine on sensory neurons in the bladder. This reduces the activity of the sensory neurons and restores normal bladder function,” Robert W. Gereau IV, PhD, professor at Washington University in St. Louis and director of the Washington University Pain Center tells GEN.
Gereau notes that one of their big questions from the beginning was whether they would be able to obtain sufficient silencing of neuronal activity coming from the bladder to impact bladder function. The device was not the concern because they knew there was more than enough light power coming from the implanted LED system. Rather, they did not know whether the viral gene therapy vector would target enough of the sensory neurons in the bladder so that turning on the light would inhibit enough of the sensory information coming from the bladder to reduce voiding. But, senior author John Rogers, PhD, professor of materials science and engineering, biomedical engineering and neurological surgery at Northwestern University, tells GEN that they were surprised by the efficacy of this approach.
Rogers and Gereau envision that a reasonable prototype could be available within a couple of years, but, that there are some key next steps that have to be worked out. Gereau notes that, “first and foremost, a gene therapy vector suitable for use in humans will need to be developed and rigorously tested for safety.” He adds that, “this needs to provide long-term, stable expression of an inhibitor opsin that has no safety issues.” There are several ongoing gene therapy clinical trials, including some using optogenetics, so this should be achievable. “Second, we need to scale and adapt this system for use in the human bladder. We feel that this will be relatively straightforward, as the miniaturization necessary to have this closed-loop system work in a rat was a major advance here.”
Although bladder function is quite similar between rat and human, the human bladder is much larger and the tissue is thicker which could limit the ability of the light to penetrate the tissue to activate the inhibitory channels expressed in the sensory neurons with the gene therapy vector. Therefore, for human application, a different mode of light delivery may be needed. This could mean the use of red light-activated opsins and red LEDs to activate them because red light penetrates biological tissues much more efficiently. Alternatively, the light sources could be placed inside the bladder to activate the sensor neuron endings that are in the superficial cell layers inside the bladder.
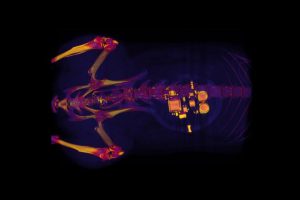
The device can be powered in a completely wireless and battery-free mode of operation due to a wireless harvesting unit that powers the entire system using near-field communication from an external secondary antenna. This powering scheme can be used in a completely battery-free mode to provide essentially limitless lifetime of operation or could be coupled with rechargeable batteries on the device for intermittent recharging by an external antenna.
Ellen Roche, PhD, assistant professor at the Institute for Medical Engineering and Science at Massachusetts Institute of Technology wrote in her accompanying News & Views article, that this work “provides a groundbreaking demonstration of how a fully closed-loop system can sense and control organ function” and it “might have major implications for efforts to alleviate organ dysfunction and to modulate pain.” Although there are hurdles to overcome, including an understanding of the body’s long-term response to a device wrapped around the bladder, Roche notes that “this type of closed-loop system might be poised to have a key role in driving a transformative shift towards the use of such strategies to treat human disease.”



